
By Dan Trencher
It’s 2019 and it’s no surprise that healthcare continues to face the seemingly uncontainable and unsustainable challenges surrounding cost and access. These challenges have too often contributed to defining care experiences over the last decade. In recent years, consumers have been shouldering more of the spending burden, and this year in the Golden State specifically, healthcare premiums for Covered California plans and those on the individual market will rise 9 percent—more than double our region’s rate of inflation.
As employees dig deeper into their pockets and employers weigh options for affordable insurance options, brokers are focusing on plans that offer a streamlined means to secure personalized, integrated care access and resolutions for medical needs. And as the world delves deeper into digital dependency, providers have responded in turn, by creating seamless online healthcare experiences that are both convenient and affordable.
Employers now demand a departure from traditional plan models in favor of solutions that generate an engaged employee pool that’s proactive, healthy, and satisfied. Mindsets are shifting, barriers are falling, and consequently, telehealth options are emerging. Make sure you’re well informed about what’s ahead as individuals forgo brick and mortar care for fingertip solutions.
- The front door to healthcare access has gone virtual
When employees first develop an illness or non-emergency health concern, they need a logical first step toward resolution beyond securing an appointment time. In a world of referring physicians, specialists, copays, and waits on hold, consumers need a clear point of entry that’s accessible on their terms and provides quality care. A virtual front door that connects them with integrated care providers is a personalized and efficient means to achieve this end.
The ability to count on high quality outcomes is also key. With general medical visits, virtual care remedies a health concern right on the spot; in other cases, the physician can help by providing a specialist recommendation right in the individual’s surrounding area, or even offer second opinion services from a top expert. As part of the full spectrum of mind-body services, physicians also respond to behavioral health needs, directing patients to these services, if needed—all through one access point, again, with proven positive outcomes.
As technology—and our willingness to use it—advances, consumers in 2019 will continue to have growing expectations of using technology for their healthcare needs. And providing a proven, guided front-door experience to your clients’ employees may be just what they’re looking for.
- Stakeholders are rethinking non-acute care
Projections indicate that by 2020, chronic diseases will account for almost three-quarters of all deaths worldwide. In California that presents a huge financial burden to employers with the latest studies indicating that over 14 million people in our state are living with at least one chronic condition and more than half of those having multiple chronic conditions. The prevalence of sedentary lifestyles and our dependence on convenience foods are increasing, heightening risks for diabetes, heart disease and obesity. As the Baby Boomers age and our society—as a whole—undergoes major demographic and economic shifts, demand for care services far outpaces the ability to meet them in brick and mortar settings.
Non-acute and chronic conditions management requires immediate attention and a model that supports organized collaboration among providers. The industry is primed for a shift in how it identifies and treats those most at-risk, especially when we consider the rise of co-morbid conditions in tandem with chronic or complex diagnoses. Virtual care will fill this gap, helping consumers navigate services to leverage both telehealth and brick and mortar care services right when they need them.
- Satisfaction and success go hand-in-hand
By providing virtual care benefits plans, California brokers and employers will generate significant improvements in user satisfaction. In the era of value-based care, it’s critical that care not only be successful and efficient, but that it’s perceived that way by both consumers and providers. The decades-long season of healthcare discontent can finally evolve into something positive—as consumers are able to navigate the care they need easily and on their terms, benefits design and accessibility will drive major improvements along the entire care continuum.
Furthermore, technology has delivered on the modern expectation for “here and now” service delivery through consumers’ mobile phones. Through grocery delivery, to ride sharing, and now healthcare, people expect convenient solutions to everyday problems. As virtual care grows, we’ll see an uptick in satisfaction levels in 2019 for healthier, more productive employees.
- No compromising for consumers
It’s no surprise that savvy consumers seek the best of both worlds. In healthcare, that means household healthcare decision-makers will demand both convenience and high-quality. In turn, employers and brokers won’t accept higher costs, but instead, will seek higher efficiencies. No compromises!
To summarize recent research from Deloitte, people want healthcare access when, where, and how it best suits them, driving behavior and services selection.
Especially as Californians’ household demographics models shift, multigenerational and multi-earner decision-makers will require an integrated, virtual care resource to maintain health and wellness support. Women, especially, who often juggle roles of employee, mom, and household “chief medical officer,” prefer sensible, seamless access to care that saves time. By offering quick resolutions to common problems and a sensible access point for more complex issues, virtual care enables true partnership with caring physicians whereby their clients’ requirements aren’t sacrificed.
- Behavioral health becomes better integrated
Thankfully, the veil of stigma and misinformation surrounding mental illness and behavioral health continues to lift. As we progress, it’s critical that behavioral services expand to more seamlessly integrate into employees’ healthcare plans. Despite nearly 70 percent of people with behavioral health problems also having a physical comorbidity, mind-body conditions are typically managed separately.
In 2019 and beyond, mental and behavioral health conditions will be managed with better outcomes through greater coordination in virtual care. Often, patients are unsure if their symptoms warrant treatment, or are unclear about what method may be best for their needs. During general telehealth visits, physicians can help individuals acknowledge and identify challenges, guiding them to secure services and further optimize the productivity and accessibility of behavioral health providers.
While some employers and brokers lean on employee assistance programs (EAPs) to meet specific individual’s needs, these services typically handle an event in isolation and in a reactive, as opposed to proactive, way. Conversely, virtual behavioral health services, through an integrated provider, enable relationship building and extended treatment–with medications when appropriate—between a patient and clinician or psychiatrist. By investing in this more proactive relationship model, healthier, happier employees will generate more productive output for employers.
- Barriers fall; virtual care momentum progresses
Virtual care has moved past the point of inevitability. As technology dependence has fueled user trends toward on-demand consumption of services, additional developments from regulatory and economic entities have aligned to ensure virtual care’s success.
Under proposed rules implementing the Bipartisan Budget Act of 2018, the Centers for Medicare & Medicaid Services (CMS) will broaden the ability for Medicare Advantage plans to include telehealth as part of their bids for the 2020 plan year. Certainly this will drive broader adoption of virtual care services and further spread to impact decision-making by commercial payers in the coming years. Likewise, state parity laws around reimbursement of telehealth services are shifting positively for virtual care’s expansion as a central point for integrated care delivery. As we look to the future, employers can expect the influence of virtual care to grow and for payment models to evolve to support it.
- AI will fulfill role as augmented intelligence
The promise of AI in healthcare is significant. It’s even more promising when we look at AI as augmented intelligence; combining the power of technology with the brightest minds in healthcare.
Through AI’s ability to mine disease, and condition-specific research, physicians can access important clinical data to make informed recommendations. One study has found that it would take a physician 29 hours each workday to keep current on the latest medical literature! Another recent publication determined that it takes an average of 17 years for new evidence-based findings to reach clinical practice.
Thankfully AI offers the ability to search, organize and consolidate medical literature at a volume and speed that no doctor could manually match. AI enables medical care to become an individualized, knowledge-rich pursuit to achieve better outcomes through the development of condition- and disease-specific solutions that are both applied personally and supported clinically.
- As access increases, costs will go down
Facts: Employers and consumers have been faced with rising insurance and medical costs, while physicians remain overworked and unable to meet demand. The consequences: patients defer both routine and specialist care, leading to the development of worsening conditions and more invasive treatments. Nearly 40 percent of Americans report skipping a recommended test or treatment, and 44 percent say they didn’t seek care for a sickness or injury in the last year because of cost.
The New Year demands a new care philosophy: let’s help employees gain affordable, timely access to all their care needs. Partnership with a full-service virtual care provider delivers this. As the high-cost of specialty medications and treatments continues to plague healthcare, the system at large must invest technologies that are proven to assure that a patient has the accurate diagnoses and subsequently the right treatment plan, minimizing unproductive care episodes and avoiding the spiraling of exorbitant costs and claims.
A centralized conception
As we quickly approach our next decade, healthcare decision-makers are considering the most effective means to integrate and streamline care episodes. California brokers, in particular, evaluate virtual benefits options on their ability to generate efficacious outcomes in a manner that leads to better outcomes.
An integrated virtual care solution enables engagement of today’s evolving consumers, and complete collaboration among care team members to address multifaceted medical concerns. Remember: healthier individuals are happier, and consequently, better, employees. The year 2019 may be the one where the stars finally align for both employers and employees to experience increased satisfaction in their health plan offerings with virtual care leading the way.
Interested in the references used for this story? Do a deeper dive here:
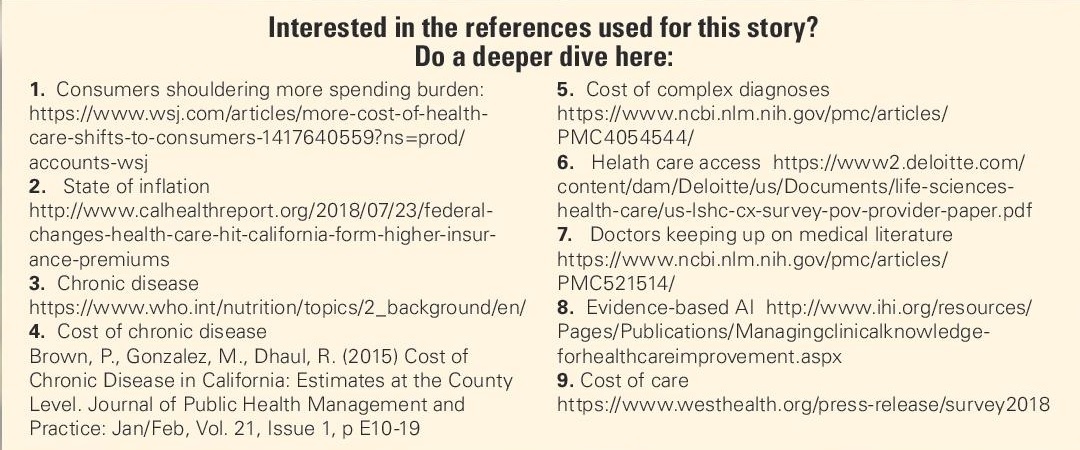 Consumers shouldering more spending burden:
Consumers shouldering more spending burden:
- State of inflation
http://www.calhealthreport.org/2018/07/23/federal-changes-health-care-hit-california-form-higher-insurance-premiums
- Chronic disease
https://www.who.int/nutrition/topics/2_background/en/
- Cost of chronic disease
Brown, P., Gonzalez, M., Dhaul, R. (2015) Cost of Chronic Disease in California: Estimates at the County Level. Journal of Public Health Management and Practice: Jan/Feb, Vol. 21, Issue 1, p E10-19
- Cost of complex diagnoses
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4054544/
- Helath care access
https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-cx-survey-pov-provider-paper.pdf - Doctors keeping up on medical literature
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC521514/
- Evidence-based AI
http://www.ihi.org/resources/Pages/Publications/Managingclinicalknowledgeforhealthcareimprovement.aspx - Cost of care
https://www.westhealth.org/press-release/survey2018
Dan Trencher is senior vice president of product & corporate strategy for Teladoc Health, Dan Trencher oversees the development and execution of new growth opportunities and products for the company, leading business initiatives that deliver compelling user experiences and transforms how people access quality care. He ensures that Teladoc Health delivers innovative commercial products, leading long-term road mapping, market analysis, product development and management, and project execution.
