 A New Strategy for Fixed Index Annuities Helps Clients if Interest Rates Rise
A New Strategy for Fixed Index Annuities Helps Clients if Interest Rates Rise
by Kenneth L. Brown • There was speculation as we rounded the corner into 2012 that interest rates could start to rise this year. But, unfortunately, the optimistic thinking did not become reality.
How Brokers Can Take Annuity Products from Commodity to Specialty
by Mark MacGillivray • Changes to the annuities marketplace require many annuity brokers to participate in specific training on product features and take continuing education credits or even adopt a new sales approach.
Balancing COBRA and Medicare
by Harry P Thal • As with most things in American life, the government plays an important role. Health insurance is no exception. Along with the laws and regulations comes alphabet soup.
Is Long Term Care Insurance a Good Buy or is it Time to Say Goodbye?
by Jack B. Schmitz, CLU ChFC CASL • Products are a good buy. Low investment returns and competition for government funds are taking a toll on alternative LTC funding strategies.
It’s Time to Educate Your Clients About Multi-Life LTCI
Douglas Hamm • The lack of a long-term care program remains a major gap in our nation’s comprehensive health care reforms
Missing Link to Financial Planning: Life Insurance
by Ron Fields • Brokers should advise clients about the value and need for voluntary insurance that can provide the added protection that employees seek.
Our Annual Dental Survey – Part III
We’ve asked the top dental providers in California to answer 28 crucial questions.
Self-Funding Concepts for the Small and Mid-Size Market The Small Market Secret
by Johnny Scharnweber, CBC • Since many agents are not familiar with this opportunity, I’m going to explain this particular segment of alternative funding for the small market.
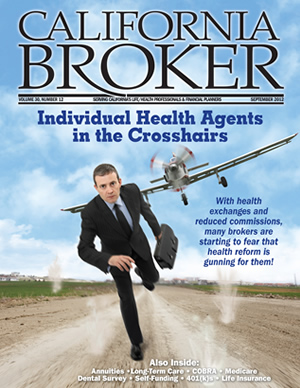
Individual Health Agents in the Cross Hairs
Are health exchanges gunning for them? Is it the end of the road?
by Leila Morris • Agents must get ready for the prospect of health insurance exchanges selling individual policies and medical loss ratio requirements driving down commissions. More people may buy insurance due to the individual mandate. However, many agents who sell individual policies are pessimistic.
Four Things Agents Need to Know About the Affordable Care Act
Robert R. Pohls, General Counsel • Insurance agents and financial advisors should recognize that they are uniquely qualified to help individuals and employers understand their obligations, evaluate their options, and develop a sensible plan for obtaining health insurance coverage on affordable terms.
COBRA Compliance – Top Issues for Employers
by Darrell Perkins • With all the new rules and regulations under health reform, fundamental and long-standing COBRA requirements still need to be addressed.
Retirement Plan Communication in an Auto-Features World
by Chuck Cornelio • The most recent solution in retirement plans is the introduction of automatic features including automatic enrollment, deferral, and escalation.
The Future of Retirement Savings
Redesigning defined contribution retirement plans to boost retirement readiness
by E. Thomas Foster Jr. •Some employers are starting to take a more proactive approach on promoting the importance of saving for retirement and making their defined contribution plans more effective and more relevant to the needs of today’s employees.
A New Strategy for Fixed Index Annuities Helps Clients if Interest Rates Rise
by Kenneth L. Brown
Historically low interest rates have been the hot discussion topic in the financial services industry in California and across the country for months. And recently, the question has been, “Just how low can they go?” There was speculation, as we rounded the corner into 2012, that interest rates could start to rise this year. But unfortunately, the optimistic thinking did not become reality.
Interest rates actually suffered a disappointing retreat, which has been particularly challenging for retirement savings options that are highly sensitive to interest rates, such as money market accounts and certificates of deposit (CDs). Traditional fixed annuity sales have struggled as well due to the continued low interest rates. In fact, total sales of fixed annuities dropped 10% in the first quarter, according to a report by LIMRA in April 2012.
There is some good news to LIMRA’s report on the annuity front: fixed index annuity sales were up 14% in the first quarter, outperforming traditional fixed annuities for the third consecutive quarter and capturing 45% of the fixed annuity market. It is fairly common knowledge that the popularity of income riders has driven sales growth, with guaranteed income emerging as a highly appealing feature to consumers. Financial professionals who are familiar with fixed index annuities were not surprised by the gains. This product category is appealing for clients who seek retirement income with a sound combination of interest-crediting flexibility and limited upside potential.
There is still a lot of confusion about fixed index annuities among financial professionals and clients in California. To help allay that, here’s a brief run-down on how fixed index annuities work: They give owners some interest-crediting potential, which is typically linked to the performance of one or more market indices. This is a big distinction from traditional fixed annuities. The owner can put all or some of the annuity’s value in the index crediting strategy and/or elect to allocate some portion to the fixed interest rate strategy that is typically offered. The owner benefits if the index performs consistently with the index crediting strategy. Yet, if the index goes down, a credit may not be received. However the owner’s principal is protected. And at every contract anniversary date, the annuity owner can re-allocate between the index and the fixed and index components of the product to seek a more appealing balance based on market conditions and personal preferences.
New Strategies That Latch Onto Rising Rates
There are willing buyers for fixed index annuities, as evidenced by LIMRA’s findings, yet many Californian financial professionals may still be wary and holding back. Interest rates on the fixed portions of these products have been disappointing. So why are people buying these products? Perhaps interest rates have been low for so long that these rates have become the new norm for many clients. Given this possibility, financial professionals must adjust their view of the interest rate hurdle and the potential sales opportunity that this product category represents.
The prospect of future rising interest rates is a major hurdle to sales of fixed annuities. It is hard to envision rates going any lower. Financial professionals and clients worry that rates will rise in the coming year or so, which makes it seem less attractive to commit now to a range of interest-rate-linked instruments, including fixed annuities.
Some insurers have introduced new features on their fixed index annuities to credit interest based on rising interest rates. Some carriers have explored using interest-rate-based crediting strategies that use a point on a published swap curve as the benchmark rate.
Another approach is a feature that provides the fixed index annuity owner with credit based upon an increase, if any, in the three-month London Interbank Offered Rate (LIBOR). The index strategy credits interest if the three-month LIBOR rises from one annuity anniversary to the next. To take advantage of this feature, clients need to have elected the strategy before interest rates rise. While we cannot predict the movement of future interest rates, it is reasonable to assume that interest rates could start to rise.
Here are the key aspects of the interest rate benchmark strategy:
• Upside Potential: If interest rates rise while the annuity owner’s funds are allocated to the interest rate benchmark strategy, the owner will earn a credit up to a cap, regardless of the performance of the equity markets during that contract year.
• Protected Principal: If the benchmark rate should drop during the contract year, the owner will receive no credit, but the annuity’s principal will be protected.
• Annual Floor Reset: The LIBOR value floor resets on each contract anniversary date, which means that the owner is in a position to accrue new credits based on interest rate increases, no matter what happened the previous year.
• Crediting Flexibility: The annuity owner is able to change the interest crediting elections on an annual basis based upon a new view of the equity and interest rate environment.
Index crediting strategies have a degree of diversification. Financial professionals can work with clients to find the right mix to adjust how much is allocated to the guaranteed rate, equity index, and interest rate benchmark, leveraging the annuity’s potential to act as a durable and flexible vehicle for retirement savings.
Debunking Annuity Myths
Myths about annuity products make clients leery and can make for a tough conversation, whether or not a fixed annuity – of any variety – may be a good fit for a particular client. A common myth is that fixed annuities have hidden fees and charges. Yet typically, there are no direct fees in the base fixed annuity. Financial professionals can dispel this myth, at the outset, in order to have a productive discussion with their clients. Generally, the only direct fees charged to a contract holder are optional features and benefits, such as guaranteed income or specific death benefits.
Another area of confusion involves surrender charges. Some California clients fear that they might face fees that would prevent them from accessing any of their funds if they needed them. In this case, a financial professional can explain to a client what surrender charges are, when they are incurred, and when money can be accessed without a surrender charge. For example, typically, an annuity owner can withdraw up to 10% of the annuity’s value in a given year without penalty. Additionally, many annuities follow the 10/10 rule, which limits surrender charges to 10 years and 10% in the first year of the annuity. Such charges diminish over time and completely disappear by the end of 10 years. Regardless of the 10/10 rule, of course, all surrender charges must be considered carefully in any situation in which a client is considering an annuity purchase.
Misunderstandings also arise when discussing limits on interest crediting in fixed index annuities, such as caps, spreads, and participation rates. Clients may think that such limits somehow boost profits for insurers. To allay this concern, a financial professional can explain that, generally, the insurance company purchases hedges to cover the cost of index credits that the annuity owner gets paid. Thus, the hedging strategy typically means that an insurer is not affected by the actual performance of the respective index and they don’t get a windfall, depending on the actual market performance or interest rate movement.
Moving Out Of the Wait and See Mode
Clients who take a wait and see approach now have a call to action with these new crediting strategies that may make a lot of sense for them. Sure, clients will still worry about stock market volatility and they express reluctance to lock into current interest rates, which may become unpalatable if rates rise in coming months. Clients may find fixed index annuities to be an appealing solution, including those with features that take advantage of rising interest rates.
It’s time to tell the real story about fixed index annuity options and address some of the negative myths that stand in people’s path. With some education and discussion of these new fixed index strategies that take advantage of rising rates, financial professionals can help their clients overcome their fear of the future and get back to saving for a more secure retirement.
–––––––––
Kenneth L. Brown is the vice president of Sales Development & Strategic Support for ING U.S. Insurance’s annuity and asset sales business, overseeing marketing, product development, regional wholesaling, sales training and development, and wholesale operations for the company’s annuity business. Before joining ING in 2005, Ken was the director of account management for CDS, a marketing and database management subsidiary of the Hearst Corporation.
Determine Suitability, Then Sell – How Brokers Can Take Annuity Products from Commodity to Specialty
by Mark MacGillivray
In 2010, the National Association of Insurance Commissioners (NAIC) adopted the updated Suitability in Annuity Transactions, Model 275. What followed were immediate and visible changes to the annuities marketplace – changes that require many annuity brokers to participate in specific training on product features and take continuing education credits or even adopt a new sales approach.
Nearly 30 states have adopted all or most of the NAICs new model regulation, which has added specific elements to the suitability requirements. The enhanced suitability rules have further emphasized the shift of annuity brokers from taking orders to being more involved in analyzing their client’s finances to better meet their needs.
Part of deviating from that commodity-based sales approach is analyzing the 12 suitability areas. This process allows a broker to gain important background information on the customer and assess suitability.
Evaluating suitability, 12 points at a time
As outlined in the NAIC model, a broker would perform a suitability analysis and collect information on 12 suitability areas:
1. Annual income: What does the customer’s financial situation look like from a monthly and annual perspective?
2. Age: Is the customer close to retiring or just starting to prepare for it? Age and stage of life matter and dictate which annuity product is the best fit.
3. Financial experience: A person with no financial experience almost always needs more help understanding the basics of investing.
4. Financial status: How much total debt does the customer have?
5. Intended use of the annuity: Each individual purchases an annuity for a different reason, with a different financial objective.
6. Financial objectives: Each individual is looking to achieve a different financial objective. For instance, ask if the customer is looking for a steady stream of income, long-term growth, or safety of principal and income.
7. Existing assets: Know which assets of a customer’s will be important in case they need to be transferred.
8. Financial time horizon: When does the customer want to accomplish their investment objective?
9. Liquidity needs: Can the customer convert their investments to cash without a substantial loss of principal?
10. Liquid net worth: Does the customer have enough liquid assets available after purchasing an annuity to cover both short- and long-term expenses?
11. Risk tolerance: Is the customer’s risk tolerance conservative, moderately conservative or aggressive? How much risk is the customer willing to take?
12. Tax status: Which status has the customer chosen when filing taxes?
Brokers collect the results from the suitability analysis and use those results as a reasonable basis to believe that the following points are true. Reason and results also inform and help in determining suitability. The consumer has been reasonably informed of the various features of the annuity, such as the following:
• Surrender charge period and amounts
• Potential tax penalties associated with a sale, exchange, surrender or annuitization of the annuity
• Expenses and investment advisory fees
• Features of and potential charges for riders
• Limitations on interest returns
• Insurance and investment components
• Market risk
• The consumer would benefit from the annuity’s features.
The annuity, as a whole, including any riders or product enhancements, is suitable for the consumer based on their suitability information. In the case of an exchange or replacement, the transaction, as a whole, is suitable.
An exchange or replacement (if applicable) is suitable taking into consideration the following, among other factors:
• Whether the consumer will incur a surrender charge or be subject to a new surrender period.
• Whether the consumer will lose existing contractual benefits.
• Whether the consumer will be subject to increased fees, investment advisory fees, or charges for riders and product enhancements.
• Whether the consumer will benefit from product enhancements and improvements.
• Whether the consumer has transacted another annuity exchange or replacement, and in particular, has had one within the preceding 36 months.
Now that brokers have the suitability process down, it is important to better understand each of the suitability areas. This article will dig deeper into these three areas:
1. Financial experience
2. Age
3. Liquid net worth
Determining a consumer’s financial experience sets the stage for the entire annuity planning process. If a consumer requires additional background and insight to make the right decision, a broker will know it up front. Additionally, the consumer’s age plays a key role in determining which type of annuity is most appropriate. Lastly, understanding the customer’s liquid net worth will provide a valuable understanding of a consumers entire financial picture.
Understanding The Customers Financial Background
Before any recommendations are given, one of the first pieces of information a broker must gather is the consumer’s financial experience. Financial experience is the knowledge that the consumer brings to the table to help determine, along with the broker, how specific financial instruments fit into an overall financial plan.
Clients with financial experience generally have a better understanding of investment basics. Those with less financial experience must rely more on the expertise of the broker and may need to take more time going over fundamental elements of annuities and financial planning.
Understanding the customer’s financial experience helps the broker know how much detail the customer will need in order to make an informed decision.
It will also identify the educational needs of the customer in order to make that informed decision.
A broker must also do their best to ensure that a customer makes an educated, informed decision. To do so, brokers must assess the financial experience of each customer and adjust their approach to making recommendations accordingly.
Applying Age and Stage Of Life
A customer’s age and stage of life can greatly affect the annuity product that a broker recommends. In many ways, a customer’s age contributes to their financial objectives and what they want and need from an annuity.
For example, individuals at retirement age generally have a lower risk tolerance. Often, these clients don’t want their savings exposed to potential market value fluctuations. At this age, clients highly value the concept of a guaranteed income for life and often look for products that offer minimum guarantees. In addition, consumers in this age bracket often need access to funds for various living expenses.
A single premium immediate annuity is often a good option for those in this stage of life. An immediate annuity guarantees payments, which start right away, for a specified time period or for a lifetime. This type of annuity is generally used as a way to generate periodic income payments. It is often used to convert accumulated savings into an income stream during retirement. Guaranteed income is important because many retirees will rely on their savings during working years to last a lifetime.
Another option for retirees is a fixed deferred annuity. Fixed deferred annuities offer tax-deferred growth in addition to principal guarantees and surrender-charge-free access to funds when qualifying events occur, such as a terminal condition or nursing home confinement. Numerous fixed deferred annuities meet these criteria. One thing to keep in mind is that the surrender charge period should not exceed the persons life expectancy.
Younger clients, who are still within their working years, are typically focused on making sure that they have sufficient funds when it is time to retire. To optimize their retirement savings, those in this age group should take advantage of certain tax-deferred investment vehicles, such as their employers 401(k), especially when they are getting free money in the form of an employer match. Once these investments are made and excess savings are still available, a fixed deferred annuity can be a viable offering because it combines safety with tax-deferred growth. A fixed deferred annuity is used primarily as a vehicle for accumulating savings and eventually distributing the value either as a payment stream or as a one-time, lump-sum payment.
Consider Liquid Assets
Brokers, not to mention state regulatory agencies, have an increased focus on client’s liquid net worth. Brokers must carry out due diligence to ensure a customer has enough liquid assets available after purchasing an annuity to cover long-term and short-term expenses. It is essential to learn if a customer has enough liquid funds to cover costs like daily living expenses or mortgage payments, as well as any money that might be needed for emergencies. Clients should not put all their liquid assets into an annuity.
State regulatory agencies are very interested in ensuring that a customer’s percentage of liquid assets used to purchase an annuity will still leave the consumer with sufficient liquid funds to handle unforeseen financial circumstances.
Carriers have often established parameters regarding the percentage of liquid assets they will accept for the customers purchase of an annuity. These parameters often fall within 25% to 40% of the customer’s liquid assets. These parameters are in place to help ensure a customer will not be left without funds should that customer lose their job or need to access emergency funds.
Find the Right Partner; Put the Wheels in Motion
With a provider’s help, an annuity broker can work through the 12 areas of suitability to help keep the financial planning focus on the customer. A provider will have the necessary tools and knowledge to help annuity brokers navigate and understand individual state regulations and therefore help determine suitability for clients. To help ensure that an annuity recommendation is compatible with the state’s suitability regulations, review the information with individual clients in mind and the state in which they do business.
Also, the right annuity provider will embody the following other qualities that help annuity brokers reach product suitability for their clients and offer support in other important areas:
• Financial stability: A provider must have financial stability. If the company goes under, the individual could lose their funds.
• Product mix: A provider should offer a variety of products so that annuity brokers can meet the needs of their clients.
• Crediting rates: It is important for an annuity broker to know the provider’s current interest crediting rates, which is equally as important as knowing the companys renewal rate history.
• Customer focus: A customer-centric provider is the key to a strong provider/broker relationship. Determine how easy it is to do business with the provider and what kind of information the provider will offer the annuity broker, including questions about its annuity products and how quickly clients can access funds.
With the support of a provider, annuity brokers can help clients embark on goal-oriented financial planning and better understand the types of annuities available to them including the one that suits them best. q
––––––––
Mark MacGillivray is a Regional Sales Director with The Standard. He has been working in the fixed annuity market for the past 17 years.
Balancing COBRA and Medicare
by Harry P Thal
Along with COBRA and Medicare laws and regulations comes alphabet soup. Many programs, created congress have become known by their acronyms. Some of the most common affecting health insurance are PPACA, HIPAA, and COBRA. And to not be out done by the federal government, California chimes in with Cal-COBRA.
First and foremost in the daily news is (PPACA), the Patient Protection and Affordable Care Act, commonly called ACA or ObamaCare. This controversial legislation has been upheld by recent Supreme Court rulings and is, therefore, the law of the land. The law is still contested by many and there is sure to be battles in more conservative states. But, for my purposes, I am going to press forward as if the law, as written, is what we must follow.
PPACA does come with a downside. All of the new benefit mandates have costs. These have been added to the monthly premiums. Almost all insurance companies are experiencing premium increases to offset the newly mandated benefits. And more are on the way. As of July, Californians will have maternity coverage added to their policies, even men and post-menopausal women!
PPACA has some other interesting characteristics that the consumer doesn’t see. One very controversial requirement is the Medical loss ratio (MLR). PPACA has determined that 85% of all group insurance premiums must be directed to medical care and 80% in the individual market. This leaves the insurance companies with 15% to 20% for all overhead. So far, this has had a minimal effect on customer service staffing and sales commissions have been reduced to meet this mandate. Insurance companies typically earn about 2% profit. What still remains a mystery is what is identified as a medical expense. Is the management of an HMO part of medical expense or administration? Time will tell as regulations are developed to administer this law.
While the states work to comply with PPACA, other letters in the soup are already part of our culture. COBRA, the Consolidated Omnibus Budget Reconciliation Act of 1984 is a federal law that requires insurance companies to continue health insurance benefits to workers and their covered dependents that are covered under their employer sponsored group plans after the worker terminates employment. This law applies to most businesses with 20 or more employees and exempts plans established by the federal government or churches that are exempt under section 501 of the Internal Revenue Code.
Dependent coverage is one of the key elements of this law. Each and every dependent who is covered under the group plan has the right to continue coverage. Therefore, if a worker retires at age 65 and goes on Medicare, the covered spouse and dependent children may remain on the group plan for the 18 months the COBRA law provides for. One comment I hear from people all the time is the high cost of COBRA. COBRA is not expensive. The monthly premium is what the employer has been paying all along for your coverage. There is a 2% billing service charge added on. That’s all! Many employees have no idea of the cost of benefits provided by their employer until they see the cost the employer had been paying.
In many instances, COBRA is used to continue insurance for inappropriate reasons. Typically it is laziness or not knowing that there may be more affordable coverage in the individual market.
Richard is retiring at age 65, leaving his 64 year old wife without coverage. While COBRA would be the answer if she could not qualify for an individual policy, Susan is a healthy person with no negative health history. She is able to buy any policy available. Since she is in good health and financially secure, she chooses a plan that is not as rich in benefits as the group plan, saving hundreds of dollars a month. She is covered if she does get sick or has a catastrophic accident or illness, and looks forward to her turning age 65.
What to do if you need coverage longer than 18 months or you work for a small business with fewer than 20 employees? California’s legislature stepped in and created Cal-COBRA, a similar bill to cover workers in the small group market. Companies with two to 19 employees fall under this law and provide similar continuation of the medical plan. Ancillary coverage, such as dental and vision, will probably not be covered, but the medical will. As previously stated, the consumer is now responsible for the full premium. In most situations the employer was paying for all or a great part of the monthly cost for the employee. In many situations, the employer may have paid for all or part of the dependent’s costs as well. Under COBRA and Cal-COBRA, the full cost of the coverage is born by the employee and covered dependents. COBRA does add a 2% administrative charge and Cal-COBRA a 10% cost.
When Cal-COBRA was enacted, it went beyond the federal COBRA legislation and provided coverage for the small employer (two to 19 employees) for 36 months. This allows the retiring person up to three years to find another position, or in many instances, wait for Medicare coverage. California law also provides for the larger employer’s terminated employee by allowing continued coverage under Cal-COBRA once the 18 months of federal COBRA runs out. This benefit is available to all covered dependents as well.
Dorothy and John get divorced. John will keep the children covered under his employer’s plan, but since Dorothy is no longer a dependent, she is no longer eligible as a spouse for continued coverage under the group plan. However, she is eligible to remain on the plan with identical medical coverage under COBRA and/or Cal-COBRA. She just needs to contact the human resources person or department at John’s employment. She will receive a new ID card and a bill each month for the next 18 or 36 months. If covered by the federal COBRA, she will need to connect with HR again in 18 months to transition to Cal-COBRA.
WARNING: COBRA and Cal-COBRA are not a substitution for Medicare. Once eligible for Medicare, you must enroll in Medicare. Do not wait past your Medicare eligibility and wait for the COBRA to run out. COBRA plans are not a substitute for Medicare, and when COBRA does run out, you will not be allowed to enroll in Medicare and will be charged a penalty (forever) once you are allowed to enroll as a late enroller. For Medicare purposes, since the employer is not paying for any part of the COBRA benefit, COBRA is considered as an individual plan. Therefore there is no special enrollment period for Medicare when coverage terminates.
Another set of letters in our alphabet soup may help consumers obtain health insurance; HIPAA.
HIPAA, the Health Insurance Portability and Accountability Act, will have different definitions, depending on whom you ask. Ask your doctor, therapist, lawyer, or banker, and they will tell you that it is a law that protects your privacy. Ask an insurance agent, and they will tell you that it guarantees you the ability to purchase health insurance even if you can’t medically qualify.
Samuel, who is 61, needed to retire early because his many medical issues didn’t allow him to perform on the job. He tried to get an individual health insurance policy when he first decided to retire, but he was unable to pass the medical underwriting requirements of the insurance plans he had applied for.
Sam needed to make his decision to elect his COBRA benefits within 63 days of the group plan’s ending. He went on COBRA and 18 months later is still unable to qualify, he took advantage of the Cal-COBRA law and continued his coverage.
Sam is now 64 and has run out his COBRA options, but still has close to a year to go before he qualifies for Medicare. He, once again, applies for an individual policy, and once again he can’t qualify medically to get accepted. His medical situation was such that the insurance company wouldn’t provide coverage, even at a higher rate. But, his health insurance agent advised him of HIPAA, which forces the insurance company to provide coverage. The insurance company must offer their two most popular selling plans to anyone who has exhausted the COBRA/Cal-COBRA benefit. The coverage must be without a break in coverage. Sam’s agent made sure that the individual health insurance application, which was rejected, stated that he wanted the HIPAA option if declined for regular coverage. Sam was offered a good plan at a costly price. As he is taking expensive medications, and really needs the coverage. He remained insured and awaits his turning age 65 and getting Medicare.
Beginning in October, 2013 most Americans will no longer need to worry about COBRA and HIPPA’s guaranteed issue since they will be able to purchase individual health insurance under the PPACA. These plans will be effective January 1, 2014. People who have financial difficulty paying for health insurance will have access to Federal assistance and will be able to purchase special health insurance policies offered by their states’ Health Insurance Exchange. Contact your local health insurance agent for more information.
–––––––––
Harry P. Thal, MA, is a licensed insurance broker in California (0621106) and other states. He is a member of the Society of Certified Senior Advisors, Past-President of the Kern Association of Health Underwriters and is on the National Assoc. of Health Underwriters (NAHU) Medicare Advisory Board. He is the recipient of the NAHU Golden Eagle Award. Harry is a Continuing Education instructor for Medicare issues with the California Association of Health Underwriters. He may be reached at 760-376-2100, e-mail harrythal@aol.com or visit him on the web at www.harrythal.com
Is LTC a Good Buy or is it Time to Say Goodbye?
by Jack B. Schmitz, CLU ChFC CASL
An attorney I met last year said she would never buy long-term care insurance (LTCI) for herself or her husband because it was not a good buy. I recently spoke with a couple whose financial planner advised them to drop their LTC policy because “she could do better” with the premium dollars. Neither of these couples had the assets to generate enough income to pay for the average monthly cost of LTC in their area, nor were they poor enough to qualify for MediCal without spending down hundreds of thousands of savings.
Insurance products are sometimes perceived as not a good buy because you spend your hard earned money on the premium and you may never receive anything in return. Paying insurance premiums and never receiving benefits is somehow perceived by many to be much worse than paying taxes for Social Security Disability or other government programs and never receiving anything.
Many LTC policyholders will get their premiums back in the form of reimbursements for eligible LTC expenses. According to the actuaries at DaVinci Consultants (they did some work for the CLASS Act program), half the people who buy a LTCI policy at age 65 and keep it in force, will use it if it has a 0-day elimination period.
With the most common 90-day elimination period, 36% will use their policy before they die. The 2012 to 2013 Sourcebook for Long Term Care Information reports that the average length of a claim has increased to 1,040 days. With $72,000 being an average number for the price of average care per year, a 1,040 day claim could cost just over $200,000. With healthcare inflation and increased demand, that number could quadruple over 30 years. For those who have cash flow and non-exempt assets between $250,000 and $5,000,000 or more, an advisor would be wise to leverage a small amount of insurance premium dollars into a large pool of LTC dollars.
A substantial amount of the LTCI policy premiums may be tax deductible and the benefits are usually tax free. Without LTC insurance, care might end up being paid with after-tax dollars. There is also the possibility of being surprised to end up in a MediCal bed on welfare, receiving the same type of care that could have been received in a private home. People who depend on the chronically ill financially or share financial resources with them, or who are otherwise emotionally and financially involved, might be surprised when $10,00 to $20,000 per month is withdrawn from assets to pay for care. Without LTC insurance, responsibility for the care and comfort of the chronically ill person becomes a bigger issue, with the burden being taken on unevenly in most cases. A long term care insurance policy can help alleviate family squabbles over the cost of care and who is providing it. Not having a policy could also result in having no advisor, no care coordinator, and no professional who is knowledgeable guidance readily available during a time of crisis.
We will be saying good bye to the current products as new products with new designs and rates are introduced. If you can still qualify for coverage, new coverage will have higher premiums for a similar potential payout. The longer you wait to buy, the higher your premium will be and the higher your probability of being declined will be as well. Underwriting is getting tougher for certain conditions as more claims data is developed. Blood test and family history will soon be used to decline more applicants. Premiums may increase as people live longer with chronic illness and claims become larger.
Say good bye to the current LTCI products, but don’t say good bye to your policy if you own one. Today’s products are a good buy for many when compared to other options. Low investment returns and competition for government funds are taking a toll on alternative LTC funding strategies.
In the future, the government may use means testing for welfare benefits, forcing more people to use previously exempt assets to pay for LTC. Filial responsibility may establish a family means testing requirement, placing an added burden on children of the chronically ill.
Today’s long term care insurance will be a good buy for those with assets that are not sufficient to provide a steady stream of income to pay for the care of a chronic illness or severe cognitive impairment. It will be a great buy for the 36+ percent who use it. If the premiums are a problem, consider a $100,000 to $250,000 starter plan to take advantage of your insurability and rates based on your current lower age.
––––––––––
Jack B. Schmitz, CLU ChFC CASL is with DI & LTC Insurance Services in San Rafael, CA 94903. He can be reached at 800-924-2294.
It’s Time to Educate Your Clients About Multi-Life LTCI
By Douglas Hamm
The Supreme Court upheld the Patient Protection and Affordable Care Act. But there is still a major gap in our nation’s comprehensive health care because there is no sustainable long-term care program. As a result of healthcare reform, businesses across the country will begin reviewing their insurance offerings and benefit packages over the next few months. This creates a unique opportunity for agents to educate clients about how adding multi-life worksite long-term care insurance (LTCI) solutions can help the bottom line.
Nearly six million U.S. employers represent mid-size workforces (those with fewer than 500 employees) making up more than half of all private-sector workers. About 70% of people will eventually need long-term care services in their lifetime; there has never been a more critical time for your clients to understand the multi-life LTCI options that are available for their workforce. Offering multi-life LTCI has great benefits for both employers and employees. Also, having more people privately insured can reduce the strain on the nation’s health care and Medicaid system. Unlike traditional group plans, multi-life LTCI plans are flexible enough for businesses of all sizes – even those with just a few employees – and program administration has never been easier. Before we discuss more of the benefits or challenges of employer-sponsored LTCI, it is important to fully understand the concept of long-term care.
What is Long-Term Care?
For a simple definition, just think care versus cure. Long-term care is needed when, due to a physical or cognitive disorder, a person is no longer able to care for themselves independently and needs ongoing assistance with activities of daily living, such as bathing, dressing, or eating without support or supervision. Therefore, long-term care generally focuses more on caring than on curing. In contrast, the general intent of health care is to restore health.
The majority of long-term care comes in the form of custodial care (helping or supporting someone perform activities of daily living) or supervisory care (providing significant supervision for a person who has a serious cognitive condition). A smaller portion of long-term care comes in the form of skilled care, such as care required from a nurse. Long-term care services may be provided in an individual’s home, in the community (adult day care), or in an assisted living or nursing home facility. LTCI can also be used for end of life services, such as hospice care. Costs of long-term care services in California can range from $51,000 annually for a home health aide, to nearly $94,000 per year for a nursing home stay with a private room, according to a recent Genworth survey. Looking at these figures, you won’t be surprised to learn that a majority of aging Americans are ill-prepared to manage the extensive costs. Additionally, many people fail to realize that government programs like Medicare and Medicaid will not fully meet their long-term care needs. Medicare only covers limited skilled care if it improves a person’s health condition. Also, no coverage is available for custodial care. Medicaid covers nursing home stays for poor and low-income citizens, which often requires a person to deplete their assets before qualifying for coverage.
Why Offer Your Clients LTCI?
The employer market is the fastest growing segment in the LTCI industry. Some mid-size employers may consider offering multi-life LTCI in response to employee demand or to increase employee recruitment and retention. Many valuable sandwich generation workers (adults who juggle the responsibilities of parents in need of assistance, as well as children still living at home), have experienced the challenges of caring for aging loved ones who were unable to prepare properly for long-term care needs. They want the opportunity to do better for themselves. Baby boomers make up about 26% of the population. It is not uncommon for businesses to have employees in this situation. Caregivers comprise much more of the workforce than most employers realize (about one in five, according to the AARP).
If your clients like to think of value in terms of dollars and cents, consider these costs:
• Businesses stand to lose up to $33.6 billion each year in lost productivity from employees’ need to care for aging loved ones.
• Employers pay 8% more for the health care of employees with eldercare responsibilities, which can cost an additional $13.4 billion per year.
• The average annual cost to employers per full-time caregiver is more than $2,100. LTCI can help employers offset some of these costs. In addition to post-retirement protection, many multi-life LTCI products offer immediate support in the form of care advisor services, which help employees manage the stress, demands, and workday distractions of caregiving. These services are designed to support, educate, and advocate for caregivers and their family members. These services also help the employer protect the interests and well-being of employees, as well as their own corporate outcomes. Multi-life programs can affect an employer’s bottom line as well. The following federal tax advantages vary by corporate status
• C-Corporations that contribute toward LTCI premiums can deduct 100% of all tax-qualified LTCI premiums as a business expense for all employees, spouses, dependents and retirees.
• S-Corporations can deduct a percentage of eligible LTCI premiums paid as a business expense.
Newer multi-life products can help small and mid-sized employers keep administration costs low, which is especially important as administration resources are typically limited.
What’s Keeping Employers Away?
If worksite programs offer obvious advantages both to employers and employees, why isn’t everyone jumping on the bandwagon? Surprisingly, most mid-size employers have not even been contacted about this benefit. It’s also important to remember that people can be misinformed about insurance products. Many employers don’t pursue LTCI for their employees due to mistaken beliefs about the challenges or barriers of LTCI, such as uncertainty about what the benefit offers, perceived administration complexity, and alleged high costs. In addition to being a great fit for both large and smaller businesses, many multi-life programs are also easy to set up thanks to streamlined processes. These include simplified underwriting, an abbreviated application process, and innovative web-based tools. Plan administration has also been simplified, which makes it easy for employers to oversee plans and access important information. As a producer, your role is to educate both employers and employees on why LTCI should be a cornerstone of their employee benefit offerings. That means sifting through the variety of products and plan options to find the best fit for your clients. A good worksite LTCI program offers a customizable plan for employers of all sizes. You need to find a product with the flexibility to suit an employer’s needs and deliver the best long-term value, such as employer-paid and voluntary, employee-paid offerings, add-ons (think inflation protection!), and varying levels of administrative support.
What’s Next?
It’s no secret that economic pressures have created a challenging environment in the LTCI market, forcing some carriers to make difficult business decisions. While the market may be adjusting, a number of carriers are committed to offering quality LTCI products and growing the industry. And the need for LTCI isn’t going anywhere. The SCAN Foundation offers the following statistics for California:
• By 2030, the number of Californians age 65 and older is projected to increase to almost 9 million, or 18% of the state’s population.
• The population of people 85 and older (those most likely needing LTC services) is expected to grow almost 40% by 2030 and 206% by 2050.
• The number of Californians age 65 and older with Alzheimer’s disease is expected to increase 38%, from 480,000 in 2010 to 660,000 in 2025.
It’s crucial for both employers and employees to understand the risks of not planning for long-term care needs, especially considering the growing demand for long-term care. For many mid-size employers, having a thoroughly researched and well-designed LTCI plan from a reliable carrier can be a smart way to provide valuable protection for both their employees and corporate goals. As an agent, it can help you find new opportunities in underserved markets and grow your book of business.
––––––––
Douglas Hamm, MBA, CLF, is vice president of Sales for LifeSecure Insurance Company LifeSecure’s insurance products are sold through a network of independent marketing organizations, brokers, and agents. For more information, e-mail dhamm@yourlifesecure.com or visit www.YourLifeSecure.com.
Missing Link to Financial Planning: Life Insurance
by Ron Fields
People work hard to establish a solid financial framework for themselves and their families with investments, home equity, savings plans, retirement accounts, and benefits. In many cases, a client wants to build a strong financial structure for the accumulated funds in order to provide for their family’s financial security well beyond the client’s death. But, like all good plans, best intentions can go awry if essential aspects of financial planning are not fully addressed.
Brokers should advise clients about voluntary insurance that can provide the added protection employees seek. Providing these benefits also helps create a robust, competitive benefit package at no direct cost to the company. With September’s focus on life insurance awareness, this is an opportune time for brokers to educate HR managers and business decision-makers about voluntary life insurance. The loss of a family member takes a toll on a family’s life emotionally. This difficult time can also create real financial challenges for the loved one’s survivors. From lost income and medical expenses to funeral costs and other accumulated bills and debt, the total financial impact can add up quickly. Brokers can help clients understand the value of educating employees about the real costs of death expenses. It will help provide families with peace of mind by planning ahead and investing in a life insurance policy.
With 35 million American households without life insurance, it is more imperative than ever for advisors to help workers understand their benefit options. Many consumers do not understand the complete scope of what is offered within a voluntary life insurance policy or the costly impact of choosing a benefit package without it.
What is a voluntary life insurance policy?
Many brokers provide voluntary life insurance policies to companies to help their employees take care of immediate and future financial needs incurred after a death. Primarily, these policies are available in two forms: term life insurance and whole life insurance. Premiums for term life insurance are fixed for a specified length of time. Premiums for whole life insurance remain the same for the policyholder’s whole life. Whole life insurance offers an investment option for funds that may be collected, borrowed, or used to pay policy premiums. This built-in cash-accumulation feature can help people pay off larger expenses, like a college education, a new car or a mortgage, allowing room for policyholders to settle debt and reach savings goals.
How does voluntary life insurance affect budgets?
A recent LIMRA study found that 34% of households admit they would immediately struggle to pay for everyday living expenses if a primary wage earner died today, underscoring how crucial life insurance coverage is for many workers.
In addition, the 2012 Aflac WorkForces Report found that 51% of workers are trying to reduce debt and 28% have less than $500 in savings for an emergency, reinforcing the importance of financial preparation for the passing of a loved one.
Family members are often left to cover both unpaid debts and new costs resulting from a death. Typical expenses include funeral bills, medical bills, and unpaid co-signed loans like those for mortgages, cars, or education. Current examples of the real cost of these expenses include the following:
• The National Funeral Directors Association found the average cost of a funeral is up to $7,755.
• According to LendingTree, the national average for a home loan is $222,261.3
• The average loan amount for a new vehicle is $25,995 and for a used vehicle is $17,050.4
What is the value of life insurance?
LIMRA research found that 12% of consumers did not buy life insurance because they could not decide what type or how much to buy. Ten percent were afraid to make the wrong decision and 8% did not know enough about life insurance to elect it. Brokers should advise HR managers and business decision-makers about the different forms of voluntary life insurance plans and how to tailor options to best meet each person’s needs.
The best time for workers to elect whole life insurance is when they’re young, while fixed premiums remain low. Whole life policies also increase their cash value over time. Since many employees cannot see the immediate benefits of a voluntary life insurance policy, it is important for brokers to highlight to employers the financial exposure workers and their families face without a policy.
Advisors should use compelling information to help employees make informed decisions about their benefit offerings. A LIMRA life insurance consumer study found that 60% of consumers do not recall being approached to buy voluntary life insurance in the last two years. In addition, 35% of shoppers who met with a sales representative did not buy voluntary life insurance because they said their sales representative failed to follow up with them.
With open enrollment season quickly approaching, this is an opportune time to help employers understand how essential it is to educate their workers about their benefit offerings, which will allow employees to make smart, cost-saving benefit choices for the coming year – decisions that could prove invaluable. Advisors should educate and promote the benefits and advantages of voluntary life insurance policies to help prepare workers for the unexpected. It will allow employees to rest easier knowing that they and their families are financially protected, even in the most difficult circumstances. Brokers and agents can elevate their status as a trusted advisor on strategic benefit decisions by giving employers the education they need to help workers make smart decisions on voluntary life insurance.
–––––––––
Ronald Fields is vice president of broker sales for Aflac. He is responsible for developing and strengthening relationships with national and regional brokers and accounts in the United States. He also oversees and coordinates the activities of Aflac market vice presidents, who are charged with increasing broker sales and market penetration in accounts with 500 or more employees. Visit aflacforbrokers.com, call 1-888-861-0251 or send an email to brokerrelations@aflac.com to learn more.
Tuning In To Our Annual Dental Survey–Part III
Welcome to Part III of California Broker’s 2012 Dental Survey. We’ve asked the top dental providers in California to answer 28 crucial questions to better help you, the agent, understand their benefits, features, and services. Read the responses and sell accordingly.
18. Do you provide coverage for all types of specialist referrals?
Aetna: Yes
Aflac: Aflac Dental does not require referrals.
Ameritas PPO and the FDH Networks: Yes, specialty coverage can be a part of any Ameritas plan designs. Our networks are comprised of a full-spectrum of specialists to cover the needs of our customers
Anthem Blue Cross: Yes, specialist care is available for both our Dental PPO and DHMO plans. No referrals are required on our Dental PPO plans, including Dental Prime and Dental Complete. On our DHMO plans, the member’s general dentist can refer them to a specialist when needed.
BEN-E-LECT: Specialist referrals are not necessary. Coverage is available for all types of specialty procedures including, but not limited to, endodontic, periodontic, cosmetic, orthodontics, oral surgery and pedodontics.
BEST Life: Yes, specialists are covered at full contract benefits as described in our Indemnity and PPO plan Certificates of Insurance. Our orthodontic plan is available for all of our PPO and Indemnity plans either at a deductible and lifetime maximum.
Blue Shield: Dental PPO/INO plan members may self-refer to any specialist, although INO members can only see network providers. For the dental HMO plan member there is no coverage for prosthodontic specialists.
Cigna: DHMO – Specialty referrals are not required for orthodontic treatment, if covered on their plan design or for pediatric care for children up to age seven as long as individuals visit network specialists. The network specialist may submit a request for pre-authorization to Cigna Dental for oral surgery and periodontal services. Individuals are responsible for the applicable patient charges listed on the Patient Charge Schedule for all covered procedures. After specialty treatment is complete, the individual should return to the network general dentist for care. If it is determined that a network specialist is not available, the general dentist will refer the patient to a non-network specialist and the patient will only be responsible for charges listed on the Patient Charge Schedule.
DPPO – Members may choose to seek service from any in- or out-of-network specialist or general dentist at any time. Of course, network dentists have agreed to our reduced fee schedules, which lower out-of-pocket expenses.
DEPO – Members can visit any network specialist or general dentist at any time to receive coverage.
Indemnity – Traditional indemnity members are always free to seek care from any licensed dentist at any time.
Delta Dental: Fee-for-service enrollees can self-refer; referral by the general dentist isn’t required. For DHMO enrollees, the primary care dentist is responsible for submitting the predetermination request and directing the enrollee to the appropriate specialist once authorization is received.
Dental Health Services: Our plans provide specialty coverage for endodontics, periodontics, oral surgery, pedodontics, and orthodontics.
Guardian: We provide coverage for all types of dental specialists.
Health Net Dental: For DHMO plans that require pre-authorization, the contracting primary care dentist completes a specialty referral form and submits to Health Net Dental. Approvals are returned to the primary care dentist, member and specialist. Upon receiving the approval, the member contacts the specialty office to schedule an appointment for completion of treatment. For plans that have direct referral, the primary care dentist may directly refer the member to a participating specialist by visiting our Website or by contacting our customer service.
Humana: Fee-for-service reimbursement encourages thorough treatment. Member complaints are reviewed by our Quality Assurance Department and through our standard grievance process.
MetLife: For Dental PPO, claims for services by licensed dental practitioners will be considered for reimbursement based on the participant’s plan design. For Dental HMO/Managed Care, the SGX and MET Series of Dental benefit plans have co-payments and/or covered percentages for endodontics, periodontics, oral surgery, pedodontics, and orthodontics services provided by a participating specialist.
Principal Financial Group: Generally yes.
Securian Dental: Our plans do not require referrals. We provide coverage based on plan benefits.
United Concordia: Our PPO plans do not require specialist referrals. Our DHMO plans require referrals for specialty coverage for endodontics, periodontics, pedodontics, oral surgery, and orthodontics. The services provided by specialists that are considered for benefit reimbursement are limited to the specifics of the dental contract for each covered member.
Western Dental: Specialty coverage is available in all of our group plans. Oral surgery, periodontics, endodontics, pedodontics, and orthodontics are covered specialties.
19. If covered, explain the process that allows the general dentist to refer to the specialist.
Aetna: For DMO plans, general practitioners can refer to a participating specialist directly based on published guidelines. DMO members have direct access to participating orthodontists and do not need a specialty referral. Indemnity and PPO plans have direct access for specialty services.
Aflac: Aflac Dental does not require referrals.
BEN-E-LECT: Referral is not necessary for any of BEN-E-LECT’s plans. The member may select a specialist and schedule an appointment upon making a phone call or personal visit.
BEST Life: No referral is necessary. Insureds can visit a specialist at any time.
Cigna: DHMO: Network general dentists initiate patient referrals for endodontic, oral surgery, and periodontal treatment. Referrals are confirmed for 90 days from the approval date. Specialty referrals are not required for orthodontic treatment or pediatric care for children up to seven years old, as long as members visit network specialists. The network specialist may submit a request for preauthorization to Cigna for oral surgery and periodontal services. Members are responsible for the applicable patient charges listed on the patient charge schedule for covered procedures. After specialty treatment is finished, the member should return to the network general dentist for care. If a network specialist is not available, the general dentist will refer the member to a non-network specialist, and the member will only be responsible for charges listed on the patient charge schedule. However, Cigna Dental Care (DHMO) network general dentists render the range of services that are required for graduation from dental school, including diagnostic treatment, preventive treatment, operative dentistry, crown and bridge, partial and complete dentures, root canal therapy, minor oral surgery, preliminary periodontal therapy, and pediatric dentistry.
DPPO: There is no need for a referral by a primary care dentist to obtain services from a specialist with the Cigna Dental PPO plan. Members may choose to seek service from any in- or out-of-network specialist or general dentist at any time. Of course, network dentists have agreed to our reduced fee schedules, which lower out-of-pocket expenses
DEPO: There is no need for a referral by a primary care dentist to obtain services from a specialist with the Cigna Dental EPO plan. Members can visit any network specialist or general dentist at any time to receive coverage.
Indemnity: Cigna Traditional indemnity members are always free to seek care from any licensed dentist at any time.
Delta Dental: Fee-for-service enrollees can self-refer; referral by the general dentist isn’t required. For DHMO enrollees, the primary care dentist is responsible for submitting the predetermination request and directing the enrollee to the appropriate specialist once authorization is received.
Dental Health Services: The general dental office sends Dental Health Services a specialist referral authorization. Upon approval, the authorization is sent back to the general dentist who informs the patient that they are now eligible to get appropriate care from a specialist
Guardian: For the DHMO plan, any complex treatment requiring the skills of a dental specialist may be referred to a Participating Specialist Dentist. Our DHMO plans offer Direct Referral in which the member may be referred directly by their primary care dentist to a participating specialist without pre-authorization.
Health Net Dental: For DHMO plans that require pre-authorization the contracting primary care dentist completes a specialty referral form and submits to Health Net Dental. Approvals are returned to the primary care dentist, member and specialist. Upon receiving the approval, the member contacts the specialty office to schedule an appointment for completion of treatment. For plans that have direct referral, the primary care dentist may directly refer the member to a participating specialist by visiting our website or by contacting our customer service.
HumanaDental: General dentists are encouraged to refer members to participating specialists to provide the highest level of benefit to the member. The general dentist can refer out-of-network if there are no specialists within a reasonable distance
MetLife: Our Dental PPO product does not require referrals for specialist care. For Dental HMO/Managed Care, the SGX and MET series of Dental benefit plans allow participating general dentists the flexibility to refer members to participating specialists without prior approval – except for orthodontic and pedodontic specialty services in CA where the member’s selected general dentist will contact us for pre-approval.
Principal Financial Group: Patients can choose any provider in the network; referrals are not required.
Securian Dental: No referral is required.
United Concordia: If a general dentist determines that a patient requires referral to a specialist, all care must be coordinated through the primary dental office. The primary dental office should refer the patient to a participating specialist located in our Concordia Plus Specialist directory and also complete the Specialty Care Referral Form. The patient should be given a copy of the referral form to give to the specialist at the time of their appointment. The specialist will then be responsible to submit the claim, corresponding documentation and referral form to United Concordia for reimbursement.
Western Dental: Once the general dentist determines that the necessary procedure is out of his or her scope of practice, the office will submit a written referral request to our plan. Western Dental’s dental director then determines whether the referral is medically necessary and whether the procedure is covered under the benefit plan.
20. Are any of your specialists board eligible/certified?
Aetna: Yes
Aflac: For benefits to be payable, the specialist must be licensed by his or her state to perform the required treatment.
BEN-E-LECT: Yes. BEN-E-LECT requires that all participating specialists be board certified.
BEST Life: All of our specialists are certified and must meet a rigorous credentialing process to be included in our network. Before a specialist can join our network, we require a license to practice, DEA/CDS certificates, Education/Training including Board Certification, work history, malpractice insurance, malpractice claims history, hospital privileges, sanctions against their license, Medicare/Medicaid sanctions, and perform ongoing monitoring of sanctions or regulatory actions. All providers must go through the credentialing process every three years.
Cigna: Yes, all network dentists contracted to provide specialty care have successfully completed post-graduate dental specialty programs in their fields. Cigna’s dental networks include specialists in periodontics, orthodontics, endodontics, pediatric dentistry and oral surgery.
It is important to note that in dentistry, board certification is not the norm. As a result, we do not require this item for credentialing. We accept dentists who are recognized specialists, including those who are board certified or board eligible.
Delta Dental: Delta Dental requires board certification where it is required by state law. Under the fee-for-service plans, Delta Dental credentials all of its participating specialists in the same manner, whether they are board-eligible or board-certified. Under the DHMO plans, Delta Dental requires all DeltaCare USA network specialists to be board-qualified.
Dental Health Services: The majority of our dental specialists are board certified.
Guardian: Many of our PPO specialists are board certified or eligible and all of the DHMO specialists are board-eligible.
Health Net Dental: Yes.
HumanaDental: All participating specialists must provide copies of their specialty licenses or residency certificates.
MetLife: In order to participate with the Dental PPO or HMO/Managed Care, specialists must submit and keep current any certifications and/or other factors necessary to maintain their specialty.
Principal Financial Group: Yes. All specialists are required to be board-eligible, board certified or be a designated specialist by the ADA.
Securian Dental: 100% of the specialists in our network are board certified or board eligible.
United Concordia: Yes, as part of our credentialing process, we verify each dentist’s education, license and certifications.
Western Dental: All contracted specialists are board-eligible/certified.
21. How do you fund your specialty care?
Aetna: Specialty services are paid on a fee–for-service basis.
Aflac: Aflac Dental insurance* pays a set amount per procedure based on a table of allowances. Additionally, policyholders have the freedom to choose their own provider without precertification. *Policies may not be available in all states. Benefits are determined by state and plan level selected. Refer to the policy for complete details, limitations, and exclusions. Coverage is underwritten by American Family Life Assurance Company of Columbus. In New York, coverage is underwritten by American Family Life Assurance Company of New York
BEST Life: Specialty care is built into the premium. Specialty care received by a network provider is reimbursed at a discounted fixed fee schedule. Specialty care received by a non-network provider is reimbursed on what is usual and customary for that area, procedure and specialty
Cigna: DHMO and DPPO specialists are compensated similarly through discounted fee-for-service, which is paid from a portion of the overall collected premiums.
Delta Dental: Specialty care is built into the premium. Under the fee-for-service plans, specialists are reimbursed by a combination of maximum plan allowances by procedure (contracted fees between Delta Dental and dentists) and coinsurance paid by the covered enrollee. Under the DHMO plan, network specialists are reimbursed for preauthorized services on a per claim basis according to contracted fee schedule and co-payment paid by the enrollee.
Dental Health Services: Specialty care and treatment is paid for on a contracted basis and payment varies by procedure. These costs are built into each plan’s monthly premium rate.
Guardian: Our PPO specialists are paid on a fee-for-service basis. For our DHMO plans, specialty care is funded through a portion of premium.
Health Net Dental: For our DHMO and DPPO plans, we underwrite and rate dental plans based on an assumed specialty care claims liability and build an allowance into our dental premiums.
HumanaDental: Specialists are paid on a fee-for-service basis according to a contracted fee-schedule amount or by reimbursement limit.
MetLife: For Dental PPO and HMO/Managed Care, specialists are reimbursed based on a predetermined fixed fee schedule. The SGX and MET Series of dental plans have co-payments and/or covered percentages for specialty services – listed on the Schedule of Benefits for the plan.
Principal Financial Group: Through normal plan provisions.
Securian Dental: Network dentists (general and specialty dentists) are reimbursed on the basis of a discounted fixed fee schedule. Network dentists agree to accept the fee schedule amount as full consideration, less applicable deductibles, coinsurance and amounts exceeding the benefit maximums and will not balance bill the member.
United Concordia: To fund specialty care, we use standard transfer business techniques to create group rates for new business and client-specific experience for existing business. As such, United Concordia requires claims experience when determining rates for clients with at least 200 enrolled contracts. United Concordia adjusts the prior carrier’s client-specific experience for assumed changes in-network utilization and payment levels, changes in benefits and utilization review, and projects it to the proposed policy period. We then add required administrative expenses and margins to create the required premium.
If prior carrier experience is not available, we actuarially create rates using client-specific demographics, including plan design, geographic location, prior carrier history, expected participation, and industry.
Western Dental: We incorporate into our premiums what we expect specialty care claims to be. We then pay the claims based on dental necessity and plan guidelines.
22. Does the member have to be referred by the primary dentist to the orthodontist or can he or she self-refer?
Aetna: The member can self-refer.
Aflac: Aflac Dental does not require referrals. Policyholders may self-refer.
BEN-E-LECT: Members may self-refer to any orthodontist they prefer. In-network versus out-of-network and plan selection will determine coverage provided.
BEST Life: No referral is necessary on our PPO or Indemnity plans.
Cigna: None of our plans require a referral for orthodontic care.
Delta Dental: Under the fee-for-service plans, enrollees can self-refer. For DHMO plans, the assigned network dentist submits a referral request for orthodontic treatment to Delta Dental. The network dentist is notified upon approval and is responsible for advising the DeltaCare USA enrollee who then contacts the assigned network orthodontist for an appointment.
Dental Health Services: Members must get a referral from one of our network dentists before visiting a participating orthodontist.
Guardian: PPO members can self-refer to all types of specialty care, including orthodontia. General dentists in our DHMO network will refer the member to a Participating Orthodontist. The referral does not require plan authorization.
Health Net Dental: Our DPPO product does not require referrals for specialty or orthodontic care, so participants may self-refer. For DHMO, there are three types of specialty referral processes based on the member’s schedule of benefits. For plans that require pre-authorization, a specialty referral form must be submitted by the primary care dentist. For plans that have direct referral, the primary care dentist may directly refer the member to a participating orthodontist by visiting our website or by contacting our customer service. For plans that allow self-referral, the member may go directly to a contracted specialist by visiting our website or by contacting our customer service.
HumanaDental: In our PPO, the member can self-refer to an orthodontist.
MetLife: Our Dental PPO product does not require referrals for specialty or orthodontic care, so participants can self-refer. For Dental HMO/Managed Care in CA, orthodontic specialty services require pre-approval. The member’s general dentist will contact us for pre-approval, and once approved will contact the member with the name of a participating orthodontist.
Principal Financial Group: A member can choose to seek services from any provider.
Securian Dental: The member can self-refer.
United Concordia: Our PPO plans allow members to self-refer. Under our DHMO plans, the primary dentist determines if a specialty referral is required, regardless of the specialty.
Western Dental: The member has to be referred by the primary dentist to the orthodontist for our IPA Dental Plan. Our Western Centers-only plan allows the member to self-refer.
23. What is the time frame for processing a referral in terms of member notification and payment to the specialist?
Aetna: DMO general practitioners usually provide a member with an immediate referral. Specialty payments are made on receipt and adjudication of the claim.
Aflac: Aflac Dental does not require referrals because policyholders have the freedom to choose their own dentist without restriction.
BEN-E-LECT: Referral is not necessary. Members may call and schedule the appointment as desired.
BEST Life: No referrals are required on our Dental PPO/Indemnity plans.
Cigna: For the DHMO, typical turnaround time for specialty referrals is five days for pre-authorization and five days for payments.
Delta Dental: For fee-for-service patients, specialty care referrals are not required and payments to specialists are processed the same as for general dentists. In 2011, the average time for processing predeterminations was five days. For DHMO enrollees, preauthorizations for specialty care processed within five business days.
Dental Health Services: Emergency referrals are processed immediately. In a non-emergency situation, referrals are processed within one to two weeks. Claims are paid within two to three weeks.
Guardian: Referrals are not required under our PPO plans. For our DHMO plans, payment to the specialist is within 30 days of receipt of the claim.
Health Net Dental: The average turnaround time in processing a non-emergency referral is 48 hours and then seven to 10 business days for the EOB to be received by the member. Once the claim is submitted by the specialist, our average turnaround time in processing is 10 business days of receipt and then seven to 10 business days for specialists to receive payment in the mail. If the claim was sent electronically, it will be sooner.
HumanaDental: Most HumanaDental plans do not require a referral from a general dentist to a specialist. The member gets a higher benefit when seeing a participating dentist and specialist. In 2008, 85% of claims and 97.4% of referrals were processed within 14 calendar days.
MetLife: For Dental HMO/Managed Care, standard referrals are processed in an average of five business days for member notification and 14 business days for payment to the provider. Our Dental PPO product does not require referrals for specialty or orthodontic care
Principal Financial Group: N/A
Securian Dental: No referral is required.
United Concordia: All referrals are immediately effective. The member is instructed to provide the referral to the specialist at the time of service and the specialist files the referral with the claim. All claims, including specialist claims, mailed to United Concordia are usually processed within 14 days. Claims filed electronically are processed immediately with payment rendered during the weekly check writer cycle
Western Dental: Emergency referrals are handled within 24-hours. The turnaround for non-emergency referrals is three business days. Specialists can expect payment in 10 business days for clean claims
24. If you limit services with an annual or lifetime maximum, what does the maximum dollar amount allowed refer to?
Aetna: The maximum dollar amount refers to the total amount Aetna will pay for covered benefits.
Aflac: The annual maximum refers to the maximum amount of benefits that may be received within a policy year per covered person. Annual maximums do not apply to wellness and X-ray benefits.
BEN-E-LECT: The maximum dollar and lifetime maximum refers to all services and procedures unless specified otherwise by benefit.
BEST Life: Lifetime maximum applies to orthodontia benefits. BEST Life offers multiple choices of calendar year maximums for preventive, basic and major procedures
Cigna: For DHMO: There is no annual or lifetime maximum; For DPPO/DEPO/Dental indemnity: The maximum dollar amount refers to the maximum amount payable by Cigna for covered services rendered.
Delta Dental: Under the fee-for-service plans, the maximum dollar amount refers to the maximum dollar amount paid by the plan. Our DHMO plans do not have annual or lifetime maximums.
Dental Health Services: The majority of our prepaid plan offerings have no annual dollar maximums, although this option is available by client request. PPO plan annual maximums range from $500 to $2,000.
Guardian: The maximum refers to the total of benefit dollars actually paid for covered services incurred within the annual period, or the member’s lifetime in the case of orthodontia. With Preventive Advantage, only Basic and Major services count toward the annual maximum. We also offer an option to cover cleaning after the maximum is reached.
Health Net Dental: The maximum dollar amount is the total amount the plan will pay for covered benefits.
Humana Dental: Annual maximum refers to the maximum amount paid annually for services, excluding orthodontia. Orthodontic treatment has a lifetime maximum
MetLife: For Dental PPO, maximums affect only the total annual reimbursement amount available under a plan to an individual or family. It does not limit access to our negotiated fees for services after the maximum is exceeded.
* For Dental HMO/Managed Care, there are no calendar or lifetime maximums.
* Negotiated fees for non-covered services may not apply in all states.
Principal Financial Group: The maximum dollar amount refers to benefits paid.
Securian Dental: The annual and lifetime maximum refer to the maximum dollar amounts we will pay for covered services in a calendar year (annual maximum) or over the coverage lifetime (lifetime maximum). Our plans generally include an annual maximum for non-orthodontic covered services and a separate lifetime maximum for orthodontia.
United Concordia: DHMO plans do not have annual or lifetime maximums. PPO plan annual and lifetime maximums vary by benefit plan and refer to the total amount paid in benefits by United Concordia annually or over the member’s lifetime.
Western Dental: The Series 7 DMO plans do not have an annual or lifetime maximum.
25. How and when do you provide eligibility information to your dental offices? How can you ensure that your offices will provide services to a member if they are not on the eligibility listing and it is after regular plan hours?
Aetna: Eligibility is available to our providers 24/7 by calling our automated telephone inquiry system or by accessing the online eligibility roster. DMO providers receive eligibility rosters the first week of each month.
Aflac: Providers may verify eligibility online – aflac.com – or by calling Aflac’s Customer Service Center – 1.800.99.AFLAC. Aflac Dental does not require prequalification for treatment.
BEN-E-LECT: BEN-E-LECT’s Interactive Voice Response (IVR) system provides eligibility 24/7. The Pre-Paid product will provide services upon collecting information from the member. This information will be transferred to BEN-E-LECT’s system electronically.
BEST Life: Providers can use BEST Life’s fax back eligibility system to determine if a member is eligible, outside of normal business hours. Offices routinely check eligibility prior to appointments and have a process in place for dealing with emergency situations.
Cigna: Dentists can view eligibility information in real time by visiting our secure website for health care professionals (24/7). In addition, we send eligibility information to our DHMO general dentists on a monthly basis. The general dentist can also call the plan for automated verification for an individual who is assigned to a particular office but is not on the eligibility list. This automated system will fax the dentist a written confirmation of eligibility. There is no eligibility listing given to DPPO dentists as people can seek treatment from any DPPO network dentist at any time. If a DPPO dentist wants to verify an individual’s participation in the plan, they can check the secure website or call our toll-free number.
Delta Dental: Dental offices can verify eligibility by contacting Delta Dental via our website, calling our automated information line or speaking with a customer services representative. Under the fee-for-service plans, a patient who is not shown as eligible may be asked to pay the bill up front. The dental office would be responsible for refunding the patient their overpayment after receiving Delta Dental payment. Under the DHMO plans, in addition to verifying eligibility as listed above, network dentists also receive eligibility lists at the beginning of each month. If an enrollee is not contained in Delta Dental’s eligibility database and claims to be eligible for benefits, Delta Dental contacts the client or the client’s benefit administrator to verify eligibility. If the eligibility verification is for an enrollee who has urgent or emergency needs, our customer service representatives will extend an urgent care authorization.
Dental Health Services: Participating dental offices get eligibility rosters twice a month. If immediate eligibility is needed at any time, the dental office can call our 24-hour automated eligibility verification system or check eligibility online through our website.
Guardian: We do not provide eligibility lists for the PPO plan. Dentists can use our online self-service website, GuardianAnytime.com or call our toll-free line and receive a faxed verification of benefits from 3:00 a.m. to 8:00 p.m., Monday through Friday and from 3:00 a.m. to 1:00 p.m. on Saturday, Pacific Time. Eligibility rosters for the DHMO plan are provided to the offices twice a month, at the first of the month and the 10th of the month. Dental offices may also call our Member Services Department from 8:00 a.m. to 5:00 p.m., Monday through Friday.
Health Net Dental: Our DHMO dentists receive a monthly updated eligibility list that includes member name, member status (active, dropped, suspended or transferred), member ID number, dependent names and eligibility status, fee schedule code, group number and capitation amount, if applicable. DPPO dentists do not receive an eligibility roster since members are not required to select a primary care general dentist. Members would simply choose any network dentist (or non-participating dentist, if they desire) and schedule an appointment. DPPO and DHMO dentists can verify eligibility information via our interactive voice response system and Website, which are accessible 24-hours a day, seven days a week. Because the IVR and Web site are available 24/7 eligibility can be verified anytime regardless of whether the need occurs during business hours.
HumanaDental: Participating offices are encouraged to check eligibility before providing treatment. They can verify members and benefits by calling our toll-free customer service line or through our automated information line to get 24 hour-a-day, seven-day-a week eligibility verification.
MetLife: For Dental PPO and Dental HMO/Managed Care, MetLife has developed a multi-channel technology platform for customer service inquiries including Web, fax, or phone. Through dedicated, real-time* channels, dentists have access to the same plan information provided to employees at the time of service. Dental offices do have access to dedicated online and automated phone system benefit information services to verify eligibility and plan details at any time. Additionally, Dental HMO/Managed Care eligibility data is forwarded once a month to each participating dentist.
* Transactions are processed in real-time except when the systems are undergoing scheduled or unscheduled maintenance or interruption.
Principal Financial Group: N/A
Securian Dental: Dental offices can use a toll-free number to call customer service to verify eligibility and benefits. Dental offices can also access www.securiandental.com to verify eligibility.
United Concordia: Dentists receive monthly capitation (eligibility) reports to verify members’ eligibility. They can also access member eligibility and benefit information 24 hours a day, 7 days a week through My Patients’ Benefits available online at www.UnitedConcordia.com or by using United Concordia’s IVR system, which can be accessed by dialing our toll free Dental Customer Service phone number at (800) 332-0366.
Western Dental: Western Dental provides eligibility listings to our Staff Model Offices electronically and printed eligibility listings to our IPA Providers. This information is updated on the 1st and 15th of each month. For members who are not on the eligibility listing, we offer guaranteed capitation to our network of providers.
26. How do you handle early termination of coverage when a member is still in the middle of orthodontic treatment?
Aetna: We stop issuing our quarterly payments when the member is no longer covered.
Aflac: Benefits will cease upon termination of coverage.
BEN-E-LECT: Payment for benefits will cease at the end of the month for which the termination became effective.
BEST Life: Coverage terminates at the end of the month in which a member is no longer eligible.
Cigna: Coverage for a dental procedure that was started before disenrollment from the plan (crowns, root canal treatment, bridges, dentures, and partials if the teeth were fully prepared or the final impressions), will be extended for 90 days after disenrollment unless it was due to non-payment of premiums.
Coverage for orthodontic treatment which was started before disenrollment from the dental plan will be extended to the end of the quarter or for 60 days after disenrollment, unless it was due to non-payment of premiums.
Our standard extension of coverage is 90 days; however, other arrangements can be made.
Delta Dental: Delta Dental’s obligation to pay toward orthodontic treatment terminates following the date the enrollee loses eligibility or upon termination of the client’s contract.
Dental Health Services: If a member’s coverage is terminated in the middle of orthodontic treatment, we encourage the member to participate in a COBRA individual plan that will allow the member to retain orthodontic benefits. If the member chooses not to maintain their coverage, the dental office can prorate any additional treatment fees. The member would then only be responsible for the prorated amount of the full treatment cost.
Guardian: When an orthodontic appliance is inserted prior to the PPO member’s effective date, we will cover a portion of treatment. Based on the original treatment plan, we determine the portion of charges incurred by the member prior to being covered by our plan and deduct them from the total charges. Our payment is based on the remaining charges. We limit what we consider of the proposed treatment plan to the shorter of the proposed length of treatment, or two years from the date the orthodontic treatment started. Also, we enforce the plan’s orthodontic benefit maximum by reducing the total benefit that Guardian would pay by the amount paid by the prior carrier, if applicable. If a member is undergoing orthodontic treatment and his or her Guardian coverage terminates, we pro-rate the benefit to cover only the time period during which coverage was in force. We do not extend benefits.
Our DHMO agreement provides for the Contracted Orthodontist to complete treatment at the contracted patient charge on a number of our plans. As an additional contract rider we can allow for supplemental transfer coverage for Orthodontia under our DHMO.
HumanaDental: HumanaDental will prorate to provide the appropriate amount given during the time the member was in the plan.
MetLife: For Dental PPO and HMO/Managed Care, benefit consideration for orthodontic treatment will cease within the month that coverage terminates unless the participant obtains continuation of coverage, in which case benefits would continue as long as coverage remains in effect.
Principal Financial Group: On individual terminations, some of our plans allow for extended benefits that provide one month of additional coverage.
Securian Dental: Benefits are paid based on the services received while the member was covered by Securian Dental.
United Concordia: The extension of orthodontic coverage for DHMO and PPO plans is 60 days if payments are being made monthly. However, if payments are being made on a quarterly basis, coverage will be extended to the end of the quarter in progress or 60 days, whichever is later.
Western Dental: Western Dental has designed a termination clause to protect the member. The member does not incur any additional fees for the early termination of a provider.
27. How do you handle the additional cost of OSHA required infection control in your participating offices?
Aetna: These costs are a part of doing business.
Aflac: Since Aflac Dental does not have network requirements, policyholders can choose any dentist without restriction. It is the responsibility of the each individual dentist to meet OSHA requirements.
BEN-E-LECT: This cost is maintained by each participating office. BEN-E-LECT is not responsible for the cost.
BEST Life: OSHA costs are the responsibility of the provider.
Cigna: Typically, dentists include these costs into their overhead and we do not allow dentists to charge for this separately. For our DHMO plans, we pay an encounter fee to the dentist to help offset their added cost for OSHA-required infection control.
Delta Dental: The cost is included in regular dental office overhead. Network dentists are not contractually allowed to charge Delta Dental or its enrollees a sterilization/infection control fee.
Guardian: Most dentists have incorporated the cost of Occupational Safety and Health Administration (OSHA) requirements into the fees for services and do not charge separately. If it is the office policy to charge separately for OSHA, we do not restrict or limit the fee as long as all patients, not just the PPO patients, are charged. Since there is no CDT/ADA code for OSHA, Guardian plans do not cover such charges. Also, we do not allow participating DHMO dental offices to charge additional fees for this.
Health Net Dental: OSHA-required infection control procedures are not eligible for payment. It is industry standard to implement OSHA compliant infection control standards for all equipment, facilities and staff without a standalone fee and/or reimbursement. For those dentists who do charge a separate fee, payment is the responsibility of the patient, although a Maximum Allowable Charge (MAC) is established.
HumanaDental: Most offices have incorporated the cost of OSHA required infection control in their overall service charges. These costs would be reflected in the data used to compile fee schedules. It’s not usually a separate billable expense.
MetLife: Most dentists include these charges as part of their general overhead expenses which, in turn, are part of the fees submitted to MetLife. We use these fees as the basis for reasonable and customary data and/or for determining Dental PPO or Dental HMO/Managed Care provider fee schedules, as appropriate.
Principal Financial Group: N/A
Securian Dental: The dentist must be in compliance with OSHA required standards including:
1. Meeting OSHA guidelines for hazardous material disposal including sharps.
2. Meeting all state and local requirements for safety and health. The participating office would absorb any costs associated with fulfilling this requirement.
United Concordia: Participating dental offices include sterilization costs in their service fees. In turn, United Concordia uses these fees to determine our maximum allowable charge (MAC) and fee schedules. Through a partnership with an outside vendor, we offer participating dental offices access to discounted sterilization monitoring services.
Western Dental: Western Dental handles the additional cost of infection control in its rates and does not charge a co-payment.
28. Do you provide utilization data to your clients and brokers?
Aetna: Yes.
Aflac: Since Aflac products are individually issued, this is not applicable.
BEN-E-LECT: Yes. All data is provided at plan renewal and may be provided throughout the year by request.
BEST Life: Yes, we provide utilization information for large groups
Cigna: Typically, dentists include these costs into their overhead and we do not allow dentists to charge for this separately. For our DHMO plans, we pay an encounter fee to the dentist to help offset their added cost for OSHA-required infection control.
Delta Dental: Delta Dental provides standard utilization reports to clients and brokers on an annual basis upon request.
Dental Health Services: We provide a wide range of utilization reporting, including treatment access, specialty claims activity, and member service call activity on client or broker request.
Guardian: Our standard reports are available monthly, quarterly or annually, and include the following detail: (1) dental plan summary, (2) monthly claims review, (3) cost management, (4) top 25 CDT codes by paid amount, (5) top 25 CDT codes by frequency, (6) benefits category claims comparison, (7) network overview, (8) out-of-network submitted charge comparison, and (9) claims by membership type.
Health Net Dental: Yes, we will provide utilization data upon request for large groups.
HumanaDental: Yes, on request and within the boundaries permitted by HIPAA.
MetLife: For Dental PPO and HMO/Managed Care, brokers are provided utilization data, if requested, as part of a proposal situation. Clients have online access to their utilization data or can be provided upon request.
Principal Financial Group: Yes, based upon the request of the client and/or broker.
Securian Dental: Yes, we can provide this infomraiton to individually rated employer groups upon request.
United Concordia: Yes, utilization reporting is available to clients and brokers.
Western Dental: Yes, utilization data can be provided on request to clients and brokers for large accounts.
29. Company Contact Information:
Aflac
www.aflac.com/broker
888-861-0251
brokerrelations@aflac-com
Ameritas
dental, vision and hearing
www.ameritasgroup.com
grfieldservice@ameritas.com
800-776-9446
BEN-E-LECT
P.O. Box 7809, Visalia CA 93290.
Physical Address
5429 Avenida de los Robles, Suite A, Visalia CA 93291.
www.benelect.com.
888-886-7973, fax 559-733-2325.
BEST Life
800-210-BEST; fax: 949-553-0883
www.besthealthplans.com;
info@bestlife.com
Delta Dental:
Northern California Sales Offices
ncasales@delta.org
100 First Street
San Francisco CA 94105
fax: 415-972-8466
11155 International Drive, M/S A2S
Rancho Cordova CA 95670
fax: 916-858-0327
30 East River Park Place West, Suite 410
Fresno CA 93720
fax: 559-433-3009
Southern California Sales Offices
scasales@delta.org
17871 Park Plaza Drive, Suite 200, Cerritos CA 90703
fax: 562-924-3172
1450 Frazee Road, Suite 200, San Diego CA 92108
fax: 619-542-0269
The Guardian Life Insurance
Company of America
Joe Stefano, director,
All of Southern/Central California & Phoenix
jstefano@glic.com
800-662-646, direct line: 949-885-1720, fax 949-453-9919
Arthur Stern, regional manager,
Los Angeles District Office
astern@glic.com
800-225-3399, direct line: 310-765-2201,
fax : 310-312-3371
Gregg Holdgrafer, regional manager, San Diego District Office
gholdgra@glic.com
Main Phone : 800-769-6759 | direct line: 619-881-3502
The Guardian (continued)
fax 1: 619-296-3912
James Hill, regional manager, San Francisco District Office
jhill@glic.com
Main Phone: 800-832-9555 | direct line : 415-490-4413
fax 1: 415.788-4412
Chris Anderson, regional manager, Sacramento District Office
canderso@glic.com
Main Phone : 800-438-5853
direct line : 916-403-2326
fax 1: 916-638-0288
Metlife
David Heil, Regional director, Northern California
1255 Treat Blvd, Suite 450
Walnut Creek, CA 94597
925-658-1102
dheil@metlife.com
Doug Gehr, Regional director, Southern California
5 Park Plaza , Suite 1900
Irvine, CA 92614
949-471-2312
dgehr@metlie.com
The Principal Financial Group
711 High Street, Des Moines, IA 50392
www.principal.com
Theresa McConeghey, Assistant Vice President – Dental, Life, Vision Products
mcconeghey.theresa@principal.com
United Concordia: 1-888-884-8224
www.UnitedConcordia.com
Gregg Holdgrafer, regional manager,
San Diego District Office
gholdgra@glic.com
800-769-6759, direct line: 619-881-3502, fax: 619-296-3912
James Hill, regional manager, San Francisco District Office
jhill@glic.com
800-832-9555, direct line: 415-490-4413, fax: 415-788-4412
Chris Anderson, regional manager,
Sacramento District Office, canderso@glic.com
800-438-5853, direct line 916-403-2326, fax: 916-638-0288
Metlife
David Heil, regional director, Northern California
1255 Treat Blvd, Suite 450, Walnut Creek, CA 94597
925-658-1102
dheil@metlife.com
Doug Gehr
Regional director, Southern California
5 Park Plaza, Suite 1900
Irvine, CA 92614
949-471-2312
dgehr@metlie.com
The Principal Financial Group
711 High Street
Des Moines, IA 50392
www.principal.com
Theresa McConeghey, assistant vice president – Dental, Life, Vision Products
mcconeghey.theresa@principal.com
United Concordia
888-884-8224
www.UnitedConcordia.com
Self-Funding–The Small Market Secret
Self Funding Concepts for the Small and Mid-Size Market
by Johnny Scharnweber, CBC
With terms like “self-funded,’’ “self-insured,’’ “partially self-funded,’’ “wrapping,’’ “alternative funding,’’ “consumer driven health plans,” “bridging the gap,” are you confused yet? Not to worry since many agents are not familiar with this opportunity, I’m going to explain this particular segment of alternative funding for the small market.
Keeping current is a challenge since the group benefit market is changing rapidly. Your clients expect you to know your product and bring all available options because you are their number one source of information. The combination of increasing costs and health care reform has increased the popularity of alternative funding plans in recent years, yet they can be confusing due to their association with the self funded market. More than 80% of employees across the nation have some sort of self funded plan and don’t realize it because of the plan design and behind-the-scenes integration. Cash flow management and high risk limit self funded or partially self funded plans are appropriate to the large group market, therefore they are not a viable option for the small and midsized employee groups.
On the other hand, alternative funding is growing as third party administrators (TPA) have taken some of the same concepts and developed an option for the small and mid-size market. This option is becoming popular with carriers as we approach 2014 when they will have to compete with the exchange as it could provide better benefit for an employer.
Taking time to broaden your knowledge base and educate yourself on more products will drive you through the health care reform implementation. Like it or not, it is the law and we have to work with it.
The concept of an alternative funding plan is based on transferring an employer group benefit plan with an HMO co-pay or low deductible PPO plan to a high deductible health plan (HDHP) that generates premium savings. The employer hires a TPA to create a plan document that allows them to share some of the costs underneath the deductible portion of the HDHP. This allows employees to continue receiving benefits that are similar to the benefits they had with their former plan. Premium savings generated from the HDHP are used to pay claims and administrative costs throughout the year, leaving a potential for the group to save money overall.
When determining whether a group is going to benefit from alternative funding, risk is certainly a factor that must be calculated. The most common mistake that agents make is predetermining their client’s risk tolerance. As a general rule, health insurance brokers and agents do not deal with risk as it relates to their job. In sharp contrast, employers are constantly evaluating and calculating risk on multiple levels. It’s a good idea to present the option and let the employer make the call. We often run across an employer with a rich plan. The cost savings from transferring to the HDHP would cover the costs of the new plan’s premium as well as administrative costs and maximum claims, therefore leaving no risk in the plan at all or a guaranteed savings.
Other times, the employer may not realize as much of a savings potential so there are a couple of things to consider. The quoting and presenting process is a time for strategic planning with the employer. It is vitally important to engage employers regarding their needs and show them how to calculate the risk associated with their plan. The initial quote presentation will show the savings potential for the group over a 12-month period. No matter what the level of risk is, employers in the small market have the option to move to another carrier. This provides a safety net.
Alternative funding has many benefits. The employer can create a plan design underneath the deductible to affect the utilization of benefits. Deductibles and co-pays can be altered throughout the year to enhance health management and steer employees away from common areas of claims abuse. For example, a $500 emergency room co-pay can be written in to keep employees from heading to the ER for non-emergency related issues. In addition, the employer would have access to claims utilization reports from the TPA to determine where the claims dollars are being spent. Can you remember a small group ever receiving a claims utilization report from the insurance carrier?
Year after year, these plans offer inherent cost savings from the reduction in premium. Employers are becoming increasingly bewildered by the fact that their medical premiums are increasing 10% to 20% annually while they are not able to increase the cost of their own goods or services more than a couple of percentage points, if at all. Alternative funding plans reduce medical premiums up to 50%, therefore reallocating the savings to claims and administrative costs that are not experiencing the same increase in rates; this can provide the group with up to 30% overall savings in the first year. In fact, TPA fees on alternative funding plans have been steady with the same per employee/per month fee for the last decade. When forecasted over five years, you’re able to show how the savings potential actually increases.
The most important part of alternative funding, by far, is the presentation to the employer. It’s important to partner with someone who not only understands the product, but who can also engage, predict, answer, and address all questions that come up. Using a GA rep with this type of background is advisable because their non-captive status allows a completely unbiased evaluation to determine whether alternative funding is appropriate for your client. Presenting alternative funding plans to employers is a win-win situation for both you and your clients who are trying to keep health care affordable. Don’t be one of those agents who lost their group because they didn’t present this option.
–––––––––
Johnny Scharnweber, CBC, is account executive and alternative funding team lead at Dickerson Employee Benefits. A leading general agency in Southern California since 1965, Dickerson offers brokers back office services for underwriting, retention support, renewal services, claims resolution, individual sales and large group consulting. With a career in business and insurance consultation, Scharnweber joined Dickerson in 2011. Contact Scharnweber at 909 549-0926 or johnny@dickerson-group.com.
Individual Health Agents in the Crosshairs
by Leila Morris
Agents who sell individual health insurance have to adjust to a whole new market thanks to health reform. They must get ready for the prospect of health insurance exchanges selling individual policies and medical loss ratio requirements driving down commissions. More people may buy insurance due to the individual mandate. Also, with the new guaranteed issue rules, individual policies will be much easier to place.
However, many agents who sell individual policies are pessimistic. Forty six percent expect to sell fewer individual insurance policies in 2014; 28% expect to sell about the same number; and 17% expect to sell more, according to a recent survey by the Kaiser Family Foundation (KFF).
How the individual market shakes out will be very important because it is expected to take up a bigger share of the overall health insurance market. According to KFF researchers, “Changes in the individual insurance market could ripple across every sector of the U.S. health care delivery system. The potential for rapid expansion of this market is strong. Also, health care reform initiatives, such as health insurance exchanges and subsidies for insurance purchases by those under qualified income thresholds, could make individual coverage more prevalent than employer-sponsored group coverage.”
The individual market could get a bigger boost if Congress passes legislation to give tax breaks to those who purchase individual policies.
On January 1, 2014, states must begin operating health insurance exchanges. They can run their own exchange, as in California, or default to a federally run exchange. KFF researchers say that many factors will affect how many people will decide to purchase insurance from the exchanges, such as how efficient the enrollment processes is, how well the plans are marketed, whether there are attractive plan selections, and whether there is good customer service.
If provider reimbursement rates are low, providers may not want to contract with plans in the exchanges, which could affect consumer choice and access to providers, according to KFF researchers. Churning, driven by the change in eligibility for individuals, is expected to be a major challenge for states. Individuals will fluctuate among eligibility for Medicaid, subsidies, and no subsidy. Depending on how frequently states decide to check eligibility status, it could mean a lot of administrative work and costs. In addition, consumer choice may stimulate shopping around, which may create a churning problem for insurers and exchange operators.
Some are skeptical of just how well the government can run an exchange. Private companies are forming their own health exchanges, seizing on the opportunity to offer superior marketing and customer services.
Forty percent of agents expect that most individual health insurance policies will eventually be sold through the exchanges, while 34% expect most to be sold outside of the exchanges. Fortunately, in California, health insurance agents will be able to sell policies through the state based exchange.
More than half of insurance executives expect health insurance to be sold mainly through exchanges within five years, according to a survey by Connecture. Sixty-one percent believe that the majority of small businesses will not offer health insurance to their employees five years from now.
Agents and the California Exchange
So what is the agent’s role in the exchange? On May 21, the State of California’s Health Benefit Exchange Board recommended that health plans participating in the exchanges pay agents directly. The preliminary recommendation is for plans to continue their own commission arrangements with agents for enrolling individuals in Exchange products. Plans will also handle all administrative functions and ongoing costs associated with managing agents and resolve any payment or compliance disputes. The Board says that this option relieves the Exchange of the burden of handling agent payments. It also maintains the relationship between the health plans and the agents.
According to the board, “The California Health Benefit Exchange is exploring alternatives to ensure that agents can play an important role for enrolling consumers in qualified health plans, and potentially in the full range of new subsidized coverage options. Agents can be a valuable resource to consumers and can play a key role in the success of the Exchange.”
The Board says that the exchange would need to establish clear policies in the following areas:
• Require commission parity inside and outside the exchange: Creating parity in commission rates between sales of Exchange and non-Exchange plans reduces incentive for agents to steer consumers toward or away from the Exchange.
• Define the agent’s role with non-exchange eligibility and enrollment: One option is for agents to refer individuals to other resources for further counsel and assistance. Another option is for the agent to provide the same full scope of counsel and advice as would a Navigator, but not be compensated for this function. This arrangement would be part of the agent’s “cost of doing business,” and reflects what many agents do now, without compensation, to help individuals enroll in the Healthy Families Program.
• Defining the scope of agent training/certification: The Exchange would need to develop training for agents. Agents would still need to get exchange certification as well as training on eligibility for subsidies and Exchange coverage before being permitted to enroll consumers in Qualified Health Plans.
• Assuring consumers’ access to unbiased information: Under this option, agents would be obligated to present all product choices regardless of compensation arrangements with the plans.
The board stressed that, while agents will continue to play a pivotal role in helping many individual Californians find and enroll in health insurance coverage, their function will evolve with the many changes that will occur effective 2014 with the implementation of the Affordable Care Act.: The following are some important changes for brokers:
• Guaranteed Issue: Health insurance companies will be required to offer coverage to everyone regardless of health status and with no screening based on pre-existing conditions. Currently, one of the important roles agents play is to help consumers navigate the complex issues related to qualifying for coverage and potential coverage exclusions.
• Standardization of Essential Health Benefits: All health plans, inside and outside of the Exchange, will be required to offer at least the standard set of defined Essential Health Benefits. For consumers, there will be a far clearer set of comparable standards of covered benefits across health plans and products.
• MLR: Effective January 1, 2011, health plans in the individual market are required to spend at least 80% of the premium collected on health care services. Non-health care services include health plan administration, marketing (including payments to agents), overhead, and profit.
• New Cost Sharing and Standards for Actuarial Value: All health insurance products, inside and outside of the Exchange, will need to offer benefits based on “actuarial value” standards related to cost sharing arrangements. (Note: the Exchange is developing recommendations for potential standardization of cost-sharing arrangements for Exchange products).
• Opportunities for Premium and Cost-Sharing Subsidies: Millions of Californians will get subsidies to make health coverage more affordable. Subsidies will take the form of coverage through Medi-Cal or Healthy Families, or through tiered financial payments based on income level to support the purchase of private plan options through the Exchange.
• Responsibility to Purchase Insurance: Starting in 2014, all Californians have the obligation to participate in the health insurance marketplace. Millions will be supported with subsidies, but this community responsibility will touch large employers (101+ employees) and individuals. Starting in 2014, the fine for not having insurance will be $95 or 1% of a person’s income, whichever is greater. Then in 2015, the fine will be $325. In 2016, the fine will be $695 or 2.5% of income. After 2016, the fine will be based on the cost-of-living adjustment every year.
The Board said, “Taken together, the factors described above mean that for agents, the only certainty is that there will be substantial changes in their environment in the coming years. From the perspective of the Exchange, the certainty – is that agents need to be part of assuring millions of Californians get the coverage and care they need.
More on the Medical Loss Ratio (MLR)
Starting in 2011, insurers in the individual market have had to spend 80% of consumers’ premiums on direct care for patients and efforts to improve care quality. Since the MLR affects how much money can be used for administrative costs, traditional brokers are likely to play a smaller role in the sale of health insurance, according to a study by Deloitte. Today, consumers purchase 42% of individual insurance policies directly from the insurance company and 36% through an insurance broker, and 13% through the Internet.
According to Deloitte, carriers may decide to exit the individual insurance market if an 80% MLR hurts their ability to meet its administrative cost and profit goals. Health plans may also consolidate to lower administrative costs. Deloitte’s predictions seem to be bearing fruit as Aetna announces a merger with Coventry Healthcare.
A 2011 NAIFA survey reveals that 75% of agents have seen their commissions drop since the MLR went into effect Jan. 1, 2011. An additional 13% have been told that their commissions would be cut. Fifty-three percent say their commissions have been cut 25% or more, which includes 17% who say their commissions have been cut 50% or more.
Twenty-three percent of agents whose commissions have been cut have reduced services for their clients while 11% got out of the health insurance market altogether. Customer services will be on the chopping block for 30% of the agents if commissions remain depressed. Twenty-nine percent say they will stop serving individual health insurance clients and 18% will stop selling health insurance altogether.
Some employers may exit the market, as well, if they face additional administrative costs of complying with the Affordable Care Act (ACA), particularly in industries with high turnover, lower-wage employees, seasonal employees, students, and part-time employees, according to Deloitte. The employer penalty for not offering coverage to employees may not be big enough to induce some employers to continue offering benefits. However, since talent retention is critical to HR, employers may continue offering coverage to attract and retain top talent.
Deloitte examined possible scenarios that could affect the individual market. If individual mandate penalties are raised, the individual market would be expected to grow along with the overall health insurance market. Having higher employer penalties is likely to persuade employers to continue offering coverage, thus reducing the number of individuals purchasing coverage in the individual market. If health exchanges are delayed beyond 2014, fewer individuals may choose to purchase insurance without the exchange option. Without exchanges in place in the earlier years, fewer employers may drop coverage as no viable alternative exists.
“We anticipate that enrollment, demographics, and plan types are likely to undergo significant changes. Drivers are not limited to ACA; they also include the evolving face of employee sponsored insurance and the U.S. workforce. In addition, economic, behavioral, political, and strategic levers are expected to shape the changing insurance coverage landscape,” say Deloitte researchers.
Looking Back at Reform Efforts
One way to gauge the future is to look to the past. The Journal of Health Affairs features a paper titled “Insurance Agents: Ignored Players in Health Insurance Reform.” Researchers looked at reforms in the individual health insurance market in New Jersey in the 1990s. One thing that is different between then and now is that, until recently, policymakers largely ignored the role of agents.
Although today’s reforms have the potential to overturn the agent’s traditional role, agents have enormous power to influence how the reforms are implemented, according to researchers. Agents were seriously affected by the New Jersey reforms, but they have since played an active role in the evolution of the regulations, largely through their continued role in interpreting the insurance market and their concerted lobbying efforts.
New Jersey implemented the Individual Health Coverage Program (IHCP) in August 1993. The IHCP requires insurers to participate in the individual health insurance market in New Jersey by selling coverage in the individual market or paying an assessment to fund the reimbursable losses of carriers that do sell such coverage. The types of policies in the individual market are standardized; there are limitations on preexisting condition exclusions, and there is a minimum loss ratio of 75%.
The role of agents changed overnight when the IHCP was implemented. Most carriers lowered agent commission rates to between 4% and 5%, which led to a dramatic decline in the number of agents selling individual health insurance in New Jersey. However, the decline is difficult to quantify since many agents also sell other products to individuals as well as health insurance to small groups.
With the standardization of benefit packages consumers had less of a need for advice from agents and brokers. Also, the rating of premiums made the pricing of standard plans transparent.
However, many consumers continued to use agents. From September 1995 to May 1996, about 71% of survey respondents said they used an insurance agent; 50% used information directly from carriers through the mail or telephone conversations; and only 13% used the buyers’ guide provided by the state. Seventy percent of those who used an agent to purchase individual health insurance said the agents represented multiple carriers. Only a third said that agents were their sole source of information while another third reported multiple sources of information.
Policyholders were more likely to use an agent if they were 35 to 54, did not have a family member with poor health status, or were self- employed. Moreover, more enrollees whose previous insurance was an individual policy reported using agents (82%), compared to those whose previous insurance was group coverage, those who or were uninsured, or those who were unsure of their previous status. Also, policy holders with indemnity plans were much more likely than those with managed care plans to use agents as a source of information (80% versus 27 %.)
Agents continue to use their standing in the community to shape state health care reform, according to researchers cited in Health Affairs. As insurance issues have become increasingly complex, agents are in a strong position to explain the potential effects of regulatory changes to legislators. Agents have a strong incentive to get involved because seemingly minor changes in regulations can affect their income and responsibilities. For example, in New Hampshire in 1994, agents helped to defeat health care reform legislation, and in Florida, they preserved their role in the reformed health insurance system.
At the local level, agents also can influence public perceptions of health insurance reforms through their day-to-day contacts with the local business community. Since many people have limited experience in making choices based solely on written materials, agents may provide a vital link to a complex system of health insurance coverage.
In this round of health reform, clients will be looking to agents to navigate the changes.
–––––––––
Leila Morris is senior editor of California Broker Magazine.
Healthcare Reform – What Agents Need to Know About the Affordable Care Act
by Robert R. Pohls, General Counsel
On June 28, 2012, the Supreme Court issued its decision in a trio of cases that challenged the constitutionality of certain provisions in the Affordable Care Act. Ultimately, a majority of the justices concluded that the Act’s individual mandate was not authorized by the Commerce Clause. At the same time, though, a different majority of the justices concluded that the provision was within Congress’ power to “lay and collect taxes.” The Affordable Care Act, therefore, has survived its primary constitutional challenges.
Given its ambitious scope, the Affordable Care Act promises to have a profound effect on health insurers, employers, and virtually every American citizen. However, insurance agents and financial advisors may be affected more by the Affordable Care Act than most other Americans because they occupy a unique place in the health insurance industry. Indeed, they are consumers of health insurance. As employers, they often provide health coverage to their employees. As producers, their livelihood may depend on their ability to market health insurance to others. The creation of state-run health benefit exchanges and other changes in the health insurance marketplace may also affect their ability to succeed.
To be sure, the public remains divided in its support for the Affordable Care Act. The presidential election in November 2012 has already sparked further debate about whether to expand, contract, or otherwise change its terms substantively. Regardless of how the political winds might change the Affordable Care Act’s course, it is essential for every insurance agent and financial advisor to have an understanding of the basic changes called for in the law.
The Individual Mandate is Riddled with Exceptions
Congress reasoned that the individual mandate was necessary to counteract a pair of significant limitations on insurers’ ability to underwrite health insurance applications, which are scheduled to become effective in 2014. One, known as “guaranteed issue,” will prohibit health insurers from denying coverage to people for any reason, including their health status. The other, known as “community rating,” will prohibit health insurers from charging people more because of their health status and gender. Instead, premiums will be allowed to vary only on the basis of geographic area, age (by a three to one ratio), tobacco use (by a 1.5 to one ratio), and the number of family members covered.
The Supreme Court acknowledged that, without the individual mandate, those provisions raised a genuine risk of “adverse selection.” As Chief Justice Roberts explained,
The guaranteed-issue and community-rating reforms do not… address the issue of healthy individuals who choose not to purchase insurance to cover potential health care needs. In fact, the reforms sharply exacerbate that problem, by providing an incentive for individuals to delay purchasing health insurance until they become sick, relying on the promise of guaranteed and affordable coverage. The reforms also threaten to impose massive new costs on insurers, who are required to accept unhealthy individuals but prohibited from charging them rates necessary to pay for their coverage. This will lead insurers to significantly increase premiums on everyone.
(Roberts, C.J., pp. 16-17) The Congressional testimony had painted a far more desperate picture, suggesting that such a circumstance would cause the financial foundation supporting the health care system to fail, “in effect causing the entire health care regime to implode.” (See, Virginia v. Sebelius, 728 F.Supp.2d 768 (E.D.Va. 2010). Most insurers, therefore, had anxiously awaited the Supreme Court’s decision.
Ultimately, the Supreme Court upheld the constitutionality of the individual mandate. In turn, many Americans assume that, beginning in 2014, they must have health insurance coverage or be prepared to make a “shared responsibility payment” as part of their federal taxes. But, the individual mandate does not apply to everyone. To the contrary, the Affordable Care Act exempts several classes of individuals from the individual mandate, including illegal aliens, members of recognized Indian tribes, and certain religious sects, incarcerated people, and anyone with a coverage gap of fewer than three months. It also provides for a hardship exemption.
At the same time, the Affordable Care Act contains other provisions that effectively limit the effect of the following individual mandate to high-income individuals:
• Individuals Who Make Less than 133% of the Federal Poverty Level: These individuals are exempt from the individual mandate, so the Affordable Care Act addressed their need for health coverage by expanding Medicaid to include people who make no more than 133% of the federal poverty level. However, the Supreme Court’s decision preserved the states’ ability to choose whether to participate in that expansion of Medicaid. Individuals who make 100% to 133% of the federal poverty level may be left without coverage in states that choose not to participate.
• Individuals Who Make 133% to 400% of the Federal Poverty Level: These individuals will be eligible to get coverage through the health benefit exchanges that are scheduled to be created in 2014. They will also be eligible for premium subsidies, which are designed to ensure that their cost of doing so does not exceed 9.5% of their income.
In 2011, the federal poverty level for a family of four was $23,050. If that figure increases by just 4% per year, a family of four that makes 400% of the federal poverty level will have an income of $112,176 in 2016. That family of four’s cost of obtaining coverage through the health benefit exchanges will be capped at $10,657 per year. Premium subsidies will pay the rest, but their alternative is to make a shared responsibility payment of just $2,085.
Although the numbers are different, families earning less than 400% of the federal poverty level will face similar choices. Indeed, while subsidies will ensure that families do not use more than 9.5% of their income to pay for health coverage, the alternative will always be to make a shared responsibility payment of no more than 2.5% of their income (capped at $2,085).
• Individuals Who Make More than 400% of the Federal Poverty Level: These individuals will be subject to the individual mandate unless the cheapest plan available in a health benefit exchange costs more than 8% of their income. The Congressional Budget Office has estimated that the cheapest plan available through a health benefit exchange (providing “bronze” level coverage) will cost a family $12,000 to $15,000 per year. If the lower of those figures proves to be accurate, a family of four that makes no more than $150,000 in 2016 also would be exempt from the individual mandate.
As a practical matter, then, the individual mandate will only apply to individuals with substantial income. Logically, many of them will already have health insurance through employer-sponsored group plans. The rest will face a choice between paying something more than $12,000 per year for health insurance and making a shared responsibility payment of not more than $2,085. Therefore, whether (and to what degree) the individual mandate actually drives more Americans into the health insurance marketplace is a debatable proposition.
The Market for Employer-Sponsored Coverage May Shrink
To make “minimum essential coverage” more available to working Americans, the Affordable Care Act contains provisions that have sometimes been referred to as the “employer mandate.” Technically, those provisions do not require employers to offer health insurance coverage to their employees. Rather, they provide that large employers (with 50 or more full-time employees) will be assessed an annual fee of $2,000 per full-time employee (in excess of 30 employees) if they do not offer “minimum essential coverage.”
Many large employers may be reviewing whether it is more economical to offer minimum essential coverage to their employees or pay penalties for not doing so. Since the employer mandate only applies to large employers, some are also considering limiting their workforce to fewer than 50 full-time employees. Importantly, the baseline year for such calculations is 2013. The Affordable Care Act’s employer mandate, therefore, presents agents with a time-sensitive opportunity to remind their largest clients that the value of employer-sponsored coverage should not be measured on economic terms alone.
Large employers that choose to offer coverage will be required to enroll an employee automatically in the employer’s lowest cost premium plan if the employee does not sign up for employer coverage or opt out of coverage. However, they will be required to provide a voucher to employees with incomes below 400% of the poverty level if the employee’s share of the premium cost is 8% to 9.8% of the employee’s income. They will also be required to pay an annual fee of $3,000 for each employee who has an annual income below 400% of the federal poverty level and opts out of the employer’s plan.
Large employers can benefit from an agent’s assistance in fashioning an employer-sponsored group plan that offers coverage that is both affordable and preferable to other options.
Tax credits already give small employers (with fewer than 25 full time employees) some incentive to offer employer-sponsored group coverage and those credits are set to increase in 2014 (from as much as 35% to as much as 50%). However, individuals and employers with fewer than 100 full time employees will also be eligible to purchase health insurance through the state-run health benefit exchanges that are scheduled to be created in 2014. In addition, the Affordable Care Act provides for subsidies that may make it more economical for low-income families to get coverage through the exchanges. Collectively, then, the Affordable Care Act’s provisions may actually cause the employer-sponsored coverage market to contract by prompting many Americans to get health coverage through the exchanges.
Agents Will Face New Competition in the Exchanges
Ostensibly, to give consumers greater choices in the health insurance marketplace, the Affordable Care Act provides for government-run health benefit exchanges from which individuals and small employers (with fewer than 100 employees) can purchase insurance. Plans in the exchanges will be required to offer benefits that meet a minimum set of standards. Insurers will offer four levels of coverage that vary based on premiums, out-of-pocket costs, and benefits beyond the minimum required. They will also offer a catastrophic coverage plan.
Premium subsidies will be provided to families with incomes from 100% to 400% of the poverty level ($29,327 to $88,200 for a family of four in 2009) to help them purchase insurance through the exchanges. Cost-sharing subsidies will also be available to people with incomes from100% to 400% of the poverty level to limit their out-of pocket spending.
The Affordable Care Act acknowledges that agents and brokers can play an important role in helping individuals and employers consider the plans offered by an exchange; enroll in that plan; and apply for premium tax credits and cost-sharing reductions. [See, 42 U.S.C. ß18032(e)]. However, each exchange will establish its own rule about the role that agents and brokers can play. At the same time, the Affordable Care Act calls for the creation of a new participant in the exchange marketplace: the navigator.
Under the Affordable Care Act, navigators will have the following five duties:
1. Conduct public education activities to raise awareness of the availability of qualified health plans.
2. Distribute fair and impartial information about enrollment in qualified health plans and the availability of premium tax credits and cost-sharing reductions.
3. Facilitate enrollment in qualified health plans.
4. Refer enrollees with a grievance, complaint, or question about their health plan, coverage, or coverage determination to a consumer assistance office or ombudsman.
5. Provide information in a culturally and linguistically appropriate manner to the population being served by the exchange. The Secretary of Health and Human Services has not yet announced the precise standards with which a navigator must comply to participate in the exchanges. But the implementing regulations specifically provide that a navigator cannot receive payment from insurers. 45 C.F.R. 155.210(d). Instead, navigators will be compensated only through grants that are funded by each exchange.
Again, agents and brokers may be navigators. They may also be able to participate in the exchanges as agents or brokers. However, they cannot do both. Either way, the plans available through the exchanges will be priced in a way that enables the exchange to compensate navigators. Therefore, agents and brokers will face a competitive disadvantage if their compensation (in the form of commissions) is passed on to consumers as an additional cost of obtaining coverage through an exchange.
Medical Loss Ratios May Change How Agents are Compensated
Even while waiting for the Supreme Court’s decision, health insurers were taking steps to comply with the medical loss ratio requirements in the Affordable Care Act. In essence, the implementing regulations require health insurers to report publicly on how premium dollars are spent. They also establish standard percentages of each premium dollar that must be spent on health claims and/or quality improvement expenses: the minimum is 80% for insurers in the individual and small group market. The minimum is 85% for insurers in the large group market. If the applicable ratio is exceeded, the excess expense must be rebated to insureds. Indeed, any rebates payable for 2011 under the Affordable Care Act’s medical loss ratio provisions must be paid by August 1, 2012.
Insurers must pay numerous expenses out of the 15% to 20% of premium dollars that remain after claims and allowable expenses. Importantly, those expenses include both commissions paid to agents and brokers as well as the insurer’s profit. The Affordable Care Act, therefore, creates an undeniable tension between an insurer’s desire to be profitable and its obligation to compensate agents and brokers.
Some insurers may remain willing to count the commissions paid to its sales force as part of the 15% to 20% of premium dollars from which it must also pay for its overhead, underwriting expenses, fraud prevention/detection, employee salaries, and compliance costs. Others may conclude that the remaining portion of premium dollars leaves too little profit. If so, they may begin asking employers and individuals to pay for their agents’ and brokers’ commissions, separate and apart from the premiums they pay for health insurance coverage.
If that comes to pass, some employers and individuals may look to the exchanges as a more cost-effective alternative. Others may begin negotiating with insurers or with agents and brokers about the commissions to be paid for traditional health insurance products. In either case, the terms on which agents and brokers are compensated for their role in the health insurance marketplace may change significantly.
Conclusion
The Affordable Care Act promises to change the health insurance industry in numerous ways. Many of its most popular changes are already in effect, such as dependent coverage to age 26, no lifetime dollar limits, restricted annual dollar limits, and small business tax credits. Many of its most politically charged changes have yet to be implemented, such as the individual mandate and the employer mandate. From a practical perspective, though, many of the changes for which it calls will have a substantial effect on insurance agents and financial advisors.
As the American public prepares for those changes, insurance agents and financial advisors should recognize that they are uniquely qualified to help individuals and employers understand their obligations, evaluate their options, and develop a sensible plan for obtaining health insurance coverage on affordable terms. By acting now, they will demonstrate their value to customers and better secure their place as an essential player in the health insurance marketplace. q
–––––––––
Rob Pohls is president and general counsel of The Law Department Inc., a California law firm, which was created in 2009 for the specific purpose of assisting insurance agents and financial advisors. A veteran trial attorney with almost 25 years of experience in litigating life, health, disability and long term care insurance disputes, Rob has earned a national reputation for his distinctive ability to achieve favorable outcomes in cases that involve challenging facts and/or novel legal questions. He is equally adept at helping clients recognize legal problems before they arise, identify their options, and develop winning strategies for using the law to both manage risk and gain a competitive business advantage. As General Counsel of The Law Department Inc., Rob uses those same skills to advise, counsel and represent insurance agents and financial advisors in connection with virtually any legal problem that can arise in connection with their businesses. For more information, visit the firm’s website (www.thelawdepartment.com) or send Rob an e-mail at rpohls@thelawdepartment.com.
COBRA Compliance Top Issues for Employers
by Darrell Perkins
The business of employee benefits seems to get more complicated with every passing open enrollment season. For better or worse, healthcare reform has accelerated the number of new rules and regulations that have to be understood and communicated to employers and employees each year. However, with all the new rules and regulations, fundamental and long-standing requirements still need to be addressed.
For instance, almost all employer groups must comply with COBRA rules. Some smaller groups may administer COBRA themselves, but many employers take advantage of the expertise of a third party administrator (TPA) to administer their COBRA.
Administering COBRA, in house, may seem like a good idea for smaller employers, but it often turns out to be penny wise and pound foolish since COBRA can be very complex. If not done in accordance with various mandates, it could lead to IRS excise taxes and ERISA statutory fines. Employers could pay as much as $500,000 or 10% of an employer’s health plan costs the prior year based on the severity of the compliance issues involved.
Here are the top issues we see employers run into with COBRA administration and tips on how to manage them.
COBRA Does Not Apply to My Company
Perhaps the most fundamental issue with COBRA is whether it applies to your client. Federal COBRA applies to all companies with more than 20 employees, but it’s not as easy as it sounds. Even if your client does not have 20 employees today, they could be subject to federal COBRA if they had more than 20 employees on more than half the business days the previous calendar year.
COBRA applies to state and local government employees, as well as full- and part-time employees. Part-time employees count as a percentage of a full-time employee based on average hours worked per week. If 40 hours is considered fulltime, a part-time employee who averages 20 hours per week counts as half of a full-time employee. Full- and part-time employees of companies under common ownership may count towards the calculation of whether or not COBRA applies.
Cal COBRA is a California state law that’s similar to federal COBRA, but applies to smaller employer groups (two to 19 lives) and allows up to 36 months of coverage. A qualified beneficiary can apply for Cal COBRA for an additional 18 months after federal COBRA has ended. Cal COBRA is administered by insurance carriers; the carriers may charge up to 110% of the health plan premium.
COBRA Does Not Apply to My Health Plan
Once it has been determined that COBRA applies to your client, you must determine which health plans are COBRA eligible. COBRA applies to all employer sponsored health plans that provide medical care to employees and their dependents. Most medical, dental, and vision plans are COBRA eligible. Flexible spending accounts (FSAs), health reimbursement arrangements (HRAs), and employee-assistance programs (EAPs) are eligible if they provide medical care. COBRA does not apply to plans that do not provide medical coverage, such as group term life, short-term disability, long-term care, AD&D, and an EAP that does not provide any medical coverage. An employer sponsored plan that meets the above criteria and is offered to active employees, must also be offered to COBRA eligible employees or qualified beneficiaries.
Who Gets COBRA and When?
To be COBRA eligible, an employee must be covered under employer-sponsored benefits the day before a qualifying event. Examples of a qualifying event are the death of an employee, termination, reduction in hours, divorce or legal separation, Medicare eligibility, or loss of dependent child status. Each of these qualifying events may affect the employee, their spouse, or dependents. It is very important to know who is COBRA eligible and under which circumstances. In many ways, not offering COBRA to an eligible qualified beneficiary is just as bad as offering COBRA to an employee who is not COBRA eligible.
Domestic Partnerships and COBRA
Only covered employees, federally recognized spouses, and dependent children are considered qualified beneficiaries with independent COBRA rights, even if the state of residence recognizes same sex domestic partnerships (see Federal Defense of Marriage Act). However, an employer may choose to be more liberal and, with carrier approval, offer COBRA coverage to an employee’s domestic partner. If COBRA benefits are extended to a domestic partner, that person should have the same rights as an active employee’s domestic partner (similarly situated person). If a domestic partner’s children are covered under an employee’s health plan, they should be considered qualified beneficiaries in connection with a qualifying event.
Not Playing by the Rules
An employer or TPA must follow COBRA procedures as mandated by COBRA guidelines. Not following procedures could put a plan out of compliance and result in errors regarding which qualified beneficiaries are offered COBRA and for how long. A COBRA plan must have reasonable documented procedures for active and former employees to inform the employer or plan administrator about a qualifying event, a second qualifying event (if applicable), or Social Security Administration (SSA) determinations. For a procedure to be considered reasonable, it must be described in a summary plan description, define who should be notified, and how the notification should be provided. The summary plan description should define the content of the notice as well as any mandated time frame to deliver the notice. Finally, procedures should be established about what to do in the event of an incomplete notice.
Giving Qualified Beneficiaries Bad Information
It is not enough to simply give a qualified beneficiary the right COBRA notice at the right time. Required COBRA notices must also contain all the information mandated by COBRA notice guidelines issued 1/1/2005.
Leaving Qualified Beneficiaries In the Dark
COBRA general notice rules mandate that an employer or TPA (upon notification by an employee of a qualifying event) is required to provide qualified beneficiaries and their dependents with COBRA eligible plan information. This COBRA information must conform to guidelines issued 1/1/2005 regarding the content of COBRA notices. Some other mandated COBRA notices include a general (initial) COBRA notice, COBRA election notice, notice of unavailability, notice of early termination and employer notice of qualifying event.
Not Providing Enough Coverage
A qualified beneficiary must be given the same coverage options as other similarly situated individuals. This coverage must be the same coverage as provided before the qualified beneficiary’s qualifying event. It cannot be reduced for a qualified beneficiary or other plan participants. Plan election changes are only allowed during the employer group’s open enrollment season.
Charging the Wrong Thing
A plan administrator may charge up to 102% of the COBRA eligible plan premium charged before the qualifying event. This premium includes former employer contributions, employee contributions, and the cost to administer the plan. A plan administrator may charge up to 150% of COBRA eligible plan premium for qualified beneficiaries with a disability extension. For self-insured groups, COBRA premiums can be based on past cost or an actuarial determination of future costs.
A plan administrator must provide a qualified beneficiary with COBRA premium costs in advance for the 12-month determination period. A determination period is essentially the group’s health plan year. Premiums may be changed for a new determination period (plan year) or if the applicable health plan premium changes outside of renewal.
Insufficient Documentation
COBRA administration can be complicated due to the various rules and requirements about who should be notified of what, when they should be notified, and the requirements for the information provided in the COBRA notifications. Keeping complete and accurate documentation throughout the COBRA process is essential and can help an employer avoid many potential compliance issues. An employer or TPA should keep records of all notices sent to and received from qualified beneficiaries, as well as track all premium payments made by qualified beneficiaries to insurers
Timing Is Everything
Successful COBRA administration is all about timing. Providing the correct length of COBRA coverage based on a specific qualifying event is important. Qualified beneficiaries may want a longer COBRA coverage period while employers may want to provide a shorter COBRA coverage period to minimize their potential exposure to claims. The length of COBRA coverage is determined by mandate. Termination of employment or a reduction in hours allows for 18 months of COBRA coverage while most other qualifying events provide 36 months of COBRA coverage. In some situations, COBRA coverage may be extended or terminated early. Some examples of extended coverage would be disability, a second qualifying event, or Medicare entitlement. Some examples of a shorter COBRA coverage period would be failure by the qualified beneficiary to pay premiums, employer discontinuation of health coverage, the qualified beneficiary becomes covered by another group health plan, or a disabled qualified beneficiary is determined to be no longer disabled. Whenever COBRA is terminated before the maximum coverage period, a notice must be given to the qualified beneficiary.
Penalties
Both employers and plan administrators are subject to tax penalties for failing to properly comply with federally mandated COBRA procedures for COBRA administration. The excise tax penalty is $100 per day for non-compliance and can increase to $200 per day if more than one qualified beneficiary is affected by the same violation. Penalties increase to as much as $2,500 for each qualified beneficiary affected by failing to comply, or a total amount based on the length of the non-compliance period, whichever is less. And if the IRS finds a violation it considers to be more than just minimal, employers may be subject to a penalty up to $15,000. The maximum any employer could be taxed in a given year is $500,000 or ten percent of the health plan costs in the previous year, whichever is less.
––––––––
Darrell Perkins is vice president of Sales in Northern California for Sterling Health Services Administration. Sterling is an Oakland, CA-based company and a leading independent administrator of health savings accounts (HSA), health reimbursement arrangements (HRA), flexible spending accounts (FSA), premium only plans (POP), COBRA, Form 5500 filing, and level funding and traditional self-insurance. For more information, visit www.sterlinghsa.com and www.sterlingsia.com.
401(k)4 – Retirement Plan Communication in an Auto-Features World
by Chuck Cornelio
In recent years, retirement savings plans have evolved in ways that directly influence how plan participants save and invest. Some of the most notable changes include the introduction of catch-up contributions, increased rollover opportunities between plans, and new investment options like life cycle and target date funds — the Roth option. The most recent solution in retirement plans is the introduction of automatic features including automatic enrollment, deferral, and escalation.
Plan sponsors are increasingly adopting automatic features to enhance the effectiveness of their retirement plan design. An astounding 94% of plan sponsors who have implemented automatic features — including automatic enrollment, automatic escalation and qualified default investment alternatives (QDIAs) — generally find them to be successful in driving higher participation and deferral rates along with better investment performance, according to a recent study by Lincoln Financial.
While new retirement communication channels have emerged since the advent of auto features, they have not kept pace with cultural and generational shifts or the evolution of plan design. The study shows that only 51% of sponsors offer customized communication and only 50% have revamped communication materials since the introduction of auto-features.
Although new communication channels have emerged, the communication that is delivered to retirement plan participants has remained relatively unchanged over the past 30 years. It is critical for plan providers and sponsors to address this issue in order to keep pace with the changes and foster greater plan participant confidence and satisfaction.
A New Communications Blueprint
Like most employer-sponsored retirement plan design innovations, taking advantage of automatic solutions doesn’t mean that you can simply set it and forget it. Employees need personalized and outcomes-based retirement communication and education to help them meet their goals and boost their retirement readiness. That means moving away from education that is technical in nature, such as how to enroll or the investments offered. It involves engaging participants in a more meaningful discussions about their saving behaviors and strategies, like their future monthly retirement income, spending power, and projected retirement lifestyle.
The following points are important for plan sponsors and providers to consider as they evaluate their plans and develop communication programs to complement their plan designs.
Begin With The End In Mind
New retirement communications should follow a participant’s saving story — meaning not just the final accumulation number or even the projected retirement income number, but also potential future buying power. Encourage participants to think about retirement in tangible terms, such as monthly spending. Give relevant examples to help participants connect the dots along the way – showing incremental progress based on their personal accounts rather than generic or static data.
Foster One-On-One Communication
An outcomes-focused approach fosters the exploration of more relevant questions and considerations and leads to a meaningful, two-way dialogue. That is why an outcomes-focused approach cannot easily take place through mass communication (in print, online or during group seminars). One-on-one conversations can be extremely powerful in helping participants identify the outcomes they desire, building a plan to get there, and then tracking the actions they take to boost their retirement readiness.
Make It Personal
Because of the comprehensive and personal nature of this conversation, offering one-on-one, face-to-face communication may be the most powerful way to deliver outcomes-focused messages. This model has already shown positive results and it will continue to grow in popularity.
Focus Evolution On Content
Content is king in the world of 24-hour news cycles and web-based retirement plan education. Innovations in technology may tempt plan sponsors to use new communication channels without changing messages. Balance freshness and relevance of communication content with outcomes-focused messages, not just new channels. Personalize retirement plan communication in every channel.
Take Inventory
Once a holistic approach is in place, revisit both automatic features and communication strategies annually. Make sure to include the investment committee, human resources, benefits managers, communicators and other decision makers to evaluate the message needs.
The emerging communication blueprint is a positive trend for the retirement plan industry and one that can be mutually beneficial for plan providers, plan sponsors and, especially, plan participants. The change can help boost retirement readiness with advantages over today’s model, including more appropriate, more personal, and more motivational communication for retirement plan participants.
The numbers are in. Automatic features are highly effective. Employers that offer these features in their plans can help Americans take charge of their retirement. Along with these innovations, participants need personalized and outcomes-focused communications and education to meet their goals and help boost their retirement readiness.
–––––––––
Chuck Cornelio is president, Retirement Plan Services, Lincoln Financial Group. The Retirement Power® Automatic Features Study is based on research conducted by Brightwork Partners, LLC, for Lincoln Financial and Retirement Made Simpler. Researchers administered the survey by phone from February 8, 2012, to March 8, 2012. The research explored automatic retirement plan features from the perspective of 201 executives responsible for managing 401(k) and 403(b) retirement plans with assets of $10 million or more. Respondents had to have implemented at least one automatic feature, including qualified default investment alternatives (QDIAs), automatic enrollment and/or automatic escalation. The survey sample is nationally representative of all 401(k) and 403(b) retirement plans with assets of $10 million or more offering at least one automatic feature (approximately 12,000 plans). To learn more about the Automatic Features Study, visit www.lincolnfinancial.com/retirementpower.
401(k)4–The Future of Retirement Savings
Redesigning defined contribution retirement plans to boost retirement readiness
by E. Thomas Foster Jr.
Jefferson is arguably one of America’s greatest futurists. He conceived the spirit of America through authorship of the Declaration of Independence; envisioned westward expansion when he secured the Louisiana Purchase; and promoted the importance of higher education by founding the University of Virginia.
But what would Jefferson say about one of today’s most pressing problems: the need for Americans to prepare for a long life in retirement?
Another futurist, Ted Benna, conceived the 401(k) plan in 1978. Today, about half of Americans have access to an employer-sponsored retirement savings plan. Yet, only two in five employees take advantage of it and, of those who do, 56% have less than $25,000 saved, according to a report by the Employee Benefits Research Institute.
Clearly, it’s time for some changes. While some have criticized the dependence on defined contribution plans for retirement security, the 401(k) and its cousins, 457(b) and 403(b) plans, aren’t going away anytime soon. It’s time to fix what’s available and, in the process, to supercharge its performance.
Benevolent Benefactor
Many employers do fret about the fact that employees are not saving enough for retirement. They would make changes in their retirement savings plan if they only knew what might help. Increasingly, employers are learning about and implementing new strategies with help from financial advisors and third party administrators. Strategies that encourage greater employee participation typically boost savings rates, make it easier for lower-paid employees to find dollars for retirement savings, and help all employees create a guaranteed income in retirement that they cannot outlive.
Put It On Automatic
Automatic enrollment is one strategy that an increasing number of employers are adopting. Employers can create a plan or redesign their plan to enroll employees automatically into a 401(k) as long as plan participants are allowed to stop their contributions within 90 days of initial enrollment. The automatic contributions are determined by a default percentage and a default investment option established by the plan to address situations where no election is made. Automatic enrollment is subject to administrative requirements.
Like the settlers who staked their claims in Jefferson’s new western territories, employees who are enrolled automatically in their employer’s 401(k) tend to stay put. They discover quickly that their retirement plan contributions have less of an impact on their paycheck than they expected because contributions are taken pre-tax. More importantly, they come to appreciate being able to watch their retirement savings grow along with their financial independence.
Escalate Annually
Many retirement savers select a savings percentage and then change it whenever they see a blue moon, which is to say “never.” Too many workers contribute far too little and many don’t even set aside enough savings to take advantage of their employer’s full matching contribution, if available. With many financial experts recommending annual retirement savings of 10% or more, it’s time to push the envelope.
Increasingly, retirement savings plans that incorporate automatic enrollment are also increasing the percentage of contributions that employees make to their 401(k) each year. Typically, automatic contributions begin at about 3% and rise 1% each year automatically until they hit a predetermined level – often 10%. Of course, there are administrative requirements, such as allowing employees to opt out or stop the escalation at a specific percentage rate.
Raise the Bar
Some employers have taken a more aggressive approach to promoting the retirement savings by raising the bar to qualify for matching contributions. Today, many employers provide a 50% match on the first 6% of pay contributed by participants to their 401(k). It’s a formula that has helped generate more than $4 trillion in retirement savings. But it’s not enough.
Consider what might happen if an employer offered a 25% match on the first 12% of pay that an employee contributes. Someone earning $50,000 a year would have to contribute $6,000 to get a $1,500 match. The bottom line is that employers can encourage more retirement savings without incurring additional costs. Of course, before employers embrace such a plan, they need to consider the ability of their employees to contribute additional savings.
Give Credit
While most Americans can and should save more for retirement, some people are struggling to simply get by in a tough economy. But all is not lost because their Uncle Sam has created a program to help lower income earners put aside money for retirement. The program is called the
“Savers Credit” and it is one of the most-overlooked retirement savings incentives available.
The Savers Credit can be applied to contributions to a defined contribution plan or an IRA. The Credit can reduce the amount of federal income tax paid by individuals with incomes of not more than $28,750 if single, $43,125 if filing as head of a household or $57,500 if married and filing jointly. The rate of the Credit can be as high as 50% or as low as 10% of retirement plan contributions, depending on the participant’s income. The maximum contribution taken into account for eligibility is $2,000 for an individual or $4,000 for a married couple.
Pay for Life
A long-overlooked problem for 401(k) plan sponsors and participants is the question of what to do with retirement savings at retirement. Increasingly, plan sponsors are providing annuity options that allow employees to turn at least a portion of their savings into a guaranteed lifetime income in retirement.
A recent study by The Hartford reveals that 86% of Americans who did not have access to a guaranteed income option within their defined contribution plan view the concept as very appealing or somewhat appealing. The younger the plan participant, the greater the appeal there is of having a guaranteed income. That means that younger employees may soon be asking for guaranteed income options.
Meanwhile, the Government Accountability Office (GAO) has encouraged the use of income products in defined contribution plans, such as annuities, noting the growing risk of Americans outliving their assets as life expectancies increase. With the declining availability of defined benefit plans and the lifetime retirement income they frequently provide, a default annuity in defined contribution plans could help to promote lifetime retirement income for more plan participants, the GAO reported last year.
Retirement plan providers have stepped up to the challenge, introducing a broad spectrum of income options for retirement savings plans. The new income options typically come in one of three flavors: a fixed annuity, an annuity as part of a target date fund, or a variable annuity investment option with a guaranteed minimum withdrawal benefit.
Benna’s Baby
Ted Benna has said that he barely recognizes his invention as today’s 401(k)s. He complains that they often come with a bewildering choice of investment options that often leave plan participants paralyzed. It’s time to make a few other changes to make Ted’s brainchild more relevant for today’s retirement saving needs.
Some employers are starting to take a more proactive approach on promoting the importance of saving for retirement and making their defined contribution plans more effective and more relevant to the needs of today’s employees. A great starting point is to incorporate features, such as automatic enrollment, automatic escalation, higher contribution limits for matching contributions, promotion of the Savers Credit, and lifetime guaranteed income options.
If everyone saved as much as they should for retirement, the $4.5 trillion that’s now sitting in defined contribution plans would start to look like chicken feed. More Americans would be able to envision a more secure financial future, much like Jefferson did in expanding the nation’s borders westward. q
––––––––
E. Thomas Foster Jr., Esq., is The Hartford’s national spokesperson for qualified retirement plans. Foster works directly with broker/dealer firms and advisers to help them build their qualified retirement plan business and educate them.
